The femoral artery is a major artery located in the thigh that supplies blood to the leg. A complete blockage of the femoral artery is considered a medical emergency. Femoral artery infections are a rare complication of femoral artery catheterization and can lead to serious issues such as pseudoaneurysms. Pseudoaneurysms are false aneurysms that can develop after procedures requiring femoral artery cannulation, resulting in prolonged hospitalization and increased morbidity. Infections in the lower limbs, such as foot ulcers, may also require hospitalization, especially if they become infected and lead to gangrene.
| Characteristics | Values |
|---|---|
| Femoral artery pseudoaneurysms (PSA) | Develop in about 1% of patients undergoing procedures that require femoral artery cannulation |
| Prolong hospitalization, consuming health-care resources, and result in significant morbidity | |
| Three independent risk factors: being female, having an intervention performed, and not having a closure device used | |
| Femoral artery infection | A rare complication of femoral artery catheterization |
| Treatment: Long-term intravenous antibiotics with occasional operative arterial reconstruction | |
| Treatment: Surgical excision and autoarterial graft insertion | |
| Treatment: Antibiotics administered according to intraoperative results | |
| Occlusive peripheral arterial disease | Infections occur easily and become serious quickly |
| Foot ulcers require meticulous care to treat infection and protect the skin | |
| Medications may be given to dissolve blood clots or prevent new clots from forming | |
| In severe cases, amputation may be required |
What You'll Learn

Femoral artery pseudoaneurysms (PSA) prolong hospital stays
The femoral artery is a major artery located in the thigh that supplies blood to the leg. It is an extension of the external iliac artery in the pelvis and runs to the lower thigh, ending behind the knee.
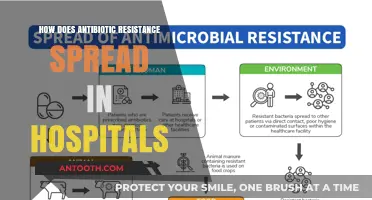
Femoral artery pseudoaneurysms (PSA or false aneurysms) are a rare complication that can develop after procedures requiring femoral artery cannulation, such as cardiac catheterization or peripheral angiography. PSA occurs in about 1% of patients undergoing these procedures and can lead to prolonged hospital stays and increased healthcare costs.
Several studies have found that patients with PSA have longer hospital stays compared to those without PSA. The presence of PSA can result in significant morbidity and increased healthcare resource consumption. In addition, certain risk factors have been identified for developing PSA, including being female, having an intervention performed, and not using a closure device during the procedure.
While surgery is an option for treating PSA, it is rarely employed due to disadvantages such as the requirement for anesthesia and the high risk of infection in the groin region. Instead, non-operative treatments such as thrombin injection and duplex-directed manual occlusion (DDMO) have gained popularity among radiologists, cardiologists, and vascular surgeons. Thrombin injection, in particular, has been suggested as the treatment of choice for femoral pseudoaneurysms due to its effectiveness and low complication rate.
In conclusion, femoral artery pseudoaneurysms (PSA) are a rare but significant complication of procedures requiring femoral artery cannulation. The development of PSA can lead to prolonged hospital stays and increased healthcare costs. However, with the exploration of non-operative treatments, such as thrombin injection, the management of PSA is becoming more efficient and effective.
Seeking Inpatient Care: Hospitalization for Depression
You may want to see also

Femoral artery infection treatment
The femoral artery is a major artery in the thigh that supplies blood to the leg. A rare complication of femoral artery catheterization is arterial infection. This can be caused by the use of percutaneous arterial closure devices, such as the Perclose device, which has been associated with a risk of severe arterial infection.
Treatment of femoral artery infections often involves long-term intravenous antibiotics and, in some cases, operative arterial reconstruction. In the case study mentioned, a patient with a methicillin-sensitive Staphylococcus aureus infection was treated with 6 weeks of intravenous cefazolin and made a full recovery.
In the case of femoral artery pseudoaneurysms (PSA or false aneurysms), which can develop after procedures requiring femoral artery cannulation, treatment options include thrombin injection and compression with a removable guidewire.
Infected pseudoaneurysms of the femoral artery can be extremely difficult to treat surgically. A case study describes the successful treatment of an infected pseudoaneurysm with surgical excision and autoarterial graft insertion.
Physicians should be aware of the potential for serious complications and the need for aggressive treatment in the event of an infection associated with femoral artery catheterization or the use of closure devices.
Hospital Internships: A Step-by-Step Guide to Success
You may want to see also

Femoral artery catheterization complications
The femoral artery is a major artery in the thigh that supplies blood to the leg. Femoral artery catheterization is a commonly used procedure, especially in cardiac catheterization. However, it is not without its complications, which can range from simple to severe, and sometimes requiring urgent hospitalization.
Femoral artery pseudoaneurysms (PSA) are a known complication, occurring in about 1% of patients undergoing femoral artery cannulation. PSAs can prolong hospitalization and result in significant morbidity. Other non-ischemic complications include arteriovenous fistulae, uncontrollable bleeding, and expanding hematoma. Acute femoral ischemia has also been observed, requiring surgical interventions such as thrombectomy and angioplasty. Chronic femoral artery occlusion can occur, leading to severe claudication, gait disturbance, or limb growth impairment.
Infection is a rare but serious complication of femoral artery catheterization. The use of percutaneous arterial closure devices, such as the Perclose device, has been associated with delayed-onset staphylococcal arterial infections requiring aggressive treatment. The incidence of septic endarteritis with the use of such devices is unknown but has been reported in a few cases.
Other complications include pituitrin-induced inguinal hematomas and pseudoaneurysms, as well as vascular complications such as peripheral vascular disease and acute blood loss through hemorrhage or acute ischemia. Efficient management of these complications is crucial for patient care.
Overall, femoral artery catheterization complications can be severe and require surgical intervention or urgent hospitalization. While some complications are rare, such as infections, others like pseudoaneurysms are more common and can lead to prolonged hospital stays.
Understanding 340B Pricing: Eligibility Criteria for Hospitals
You may want to see also

Femoral artery infection after Perclose use
The femoral artery is a major artery in the thigh that supplies blood to the leg. It is part of the body's network of arteries that deliver oxygen-rich blood from the heart to the body's tissues.
Femoral artery infections are a rare complication of femoral artery catheterization. However, there have been several reports of such infections associated with the use of the Perclose percutaneous arterial closure device. This device is used to control hemostasis after cardiac catheterization, which is a procedure used to diagnose and treat cardiovascular conditions.
In the reported cases of femoral artery infection after Perclose use, patients presented with symptoms such as right leg or groin pain, fever, and a pseudoaneurysm. One patient was a 55-year-old man with a history of hypertension and other medical conditions who underwent cardiac catheterization via the right femoral artery. Four days after the procedure, he complained of right groin pain and a fever of 104 degrees Fahrenheit. Another patient, a 50-year-old man with hypertension, underwent left heart catheterization and presented to the emergency department 19 days later with right leg pain.
Treatment for femoral artery infections associated with Perclose use typically involves aggressive treatment, including long-term intravenous antibiotics and, in some cases, operative arterial reconstruction. In the reported cases, treatment included sharp debridement of the common femoral artery, removal of the Perclose suture, and repair of the artery with saphenous vein patch angioplasty. The patients were also administered intravenous cefazolin for 6 weeks, after which they recovered uneventfully.
The incidence of septic endarteritis after Perclose use is unknown, but it is suggested that percutaneous closure devices may be associated with an increased risk of infection. Surgeons should be aware of the potential infectious complications associated with Perclose use and consider preprocedural antibiotics when using the device. While femoral artery infections requiring hospitalization are rare, they can result in prolonged hospital stays and significant morbidity.
Hospital Jobs: A Great Start for New Grads
You may want to see also

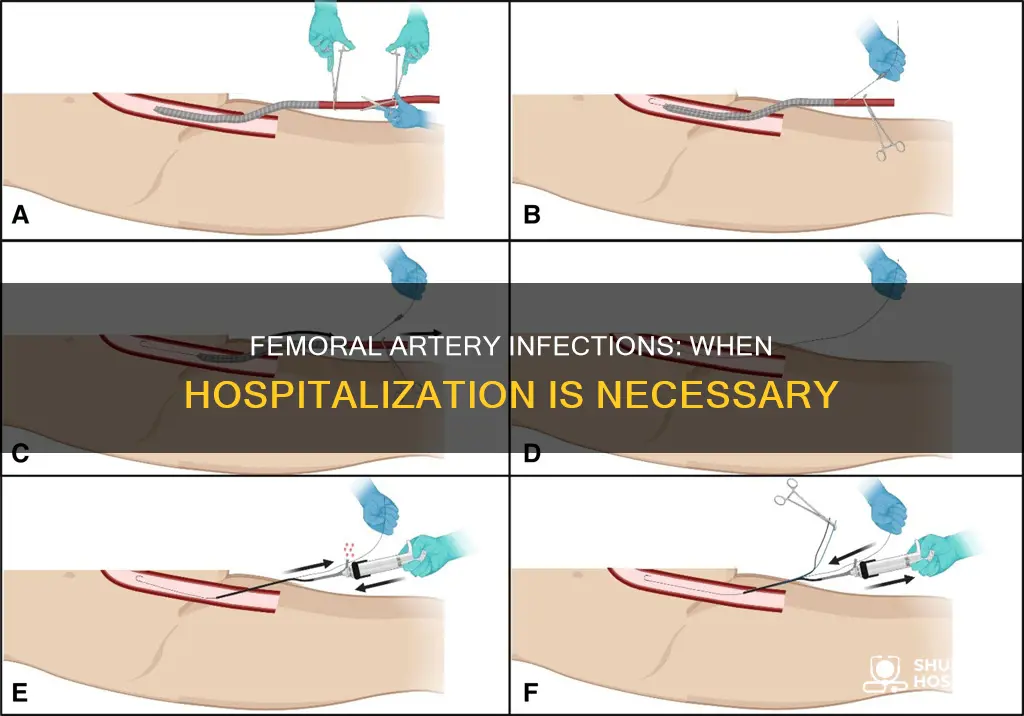
Surgical treatment for infected pseudoaneurysms
The femoral artery is a major artery in the thigh that supplies blood to the leg. A pseudoaneurysm is a "false aneurysm" that occurs when there is a breach in the arterial wall, resulting in an accumulation of blood between the layers of the artery. Pseudoaneurysms are commonly experienced vascular abnormalities that can occur in any arterial location but are most common in the femoral artery.
Infected pseudoaneurysms have a much higher risk of perforation, which can lead to significant haemorrhage if left untreated. The risk of infection is higher in IVDU patients due to the introduction of pathogens through non-sterile needles. If a pseudoaneurysm becomes infected, patients can quickly become septic, and the pseudoaneurysm becomes even more likely to rupture. Therefore, infected pseudoaneurysms require urgent surgical ligation to prevent serious complications.
Surgical repair or ligation of an infected pseudoaneurysm involves controlling the healthy artery proximal and distal to the pseudoaneurysm before opening it. The defect in the artery may then be repaired directly or with a vein or bovine patch. Ligation may also be required, but this can cause distal ischaemia and necessitate a bypass graft. Vein or bovine grafts are preferable in this case as they are more resistant to infection.
There are several non-surgical management options for pseudoaneurysms, including ultrasound-guided compression (USGC), thrombin therapy, arterial embolisation, and endovascular stent graft insertion. However, these methods are less successful for larger pseudoaneurysms, those with high-pressure flow, or in patients receiving high levels of anticoagulation.
In recent years, interventional radiological treatment methods have become the primary approach for treating pseudoaneurysms, with surgical repair now being recommended mainly for infected pseudoaneurysms, those with rapid growth, ischemia, neuropathy, or failure of previous treatments.
Managing Blood Sugar: When to Go to the Hospital
You may want to see also
Frequently asked questions
Yes, infection at the femoral artery requires immediate hospitalization. It is a medical emergency that could lead to gangrene and amputation if not treated promptly.
Symptoms of an infected femoral artery include a high fever, groin pain, and sores or ulcers that do not heal easily.
Treatment options for an infected femoral artery include long-term intravenous antibiotics, surgical debridement, and arterial reconstruction. In some cases, a thrombin injection and compression with a removable guidewire may be used.