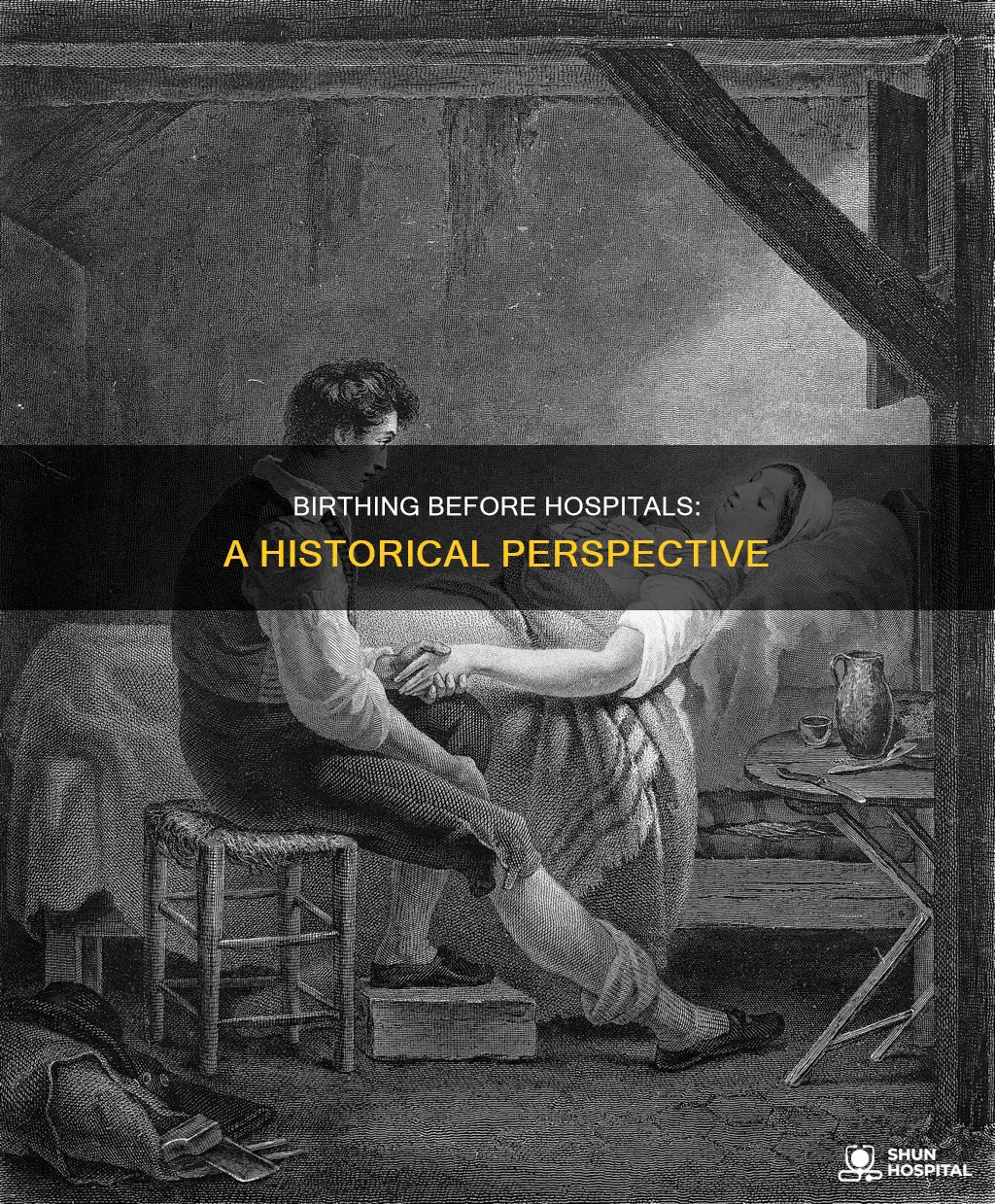
For much of human history, women gave birth at home with the help of midwives. Childbirth was often a communal affair, with female and male relatives and attendants present. In some cultures, religious figures would also be present to offer prayers for the mother's safety. The mother was often quarantined before and after childbirth. In the 18th century, forceps were invented, and men trained as physicians abroad began to return to practice in America. The shift to hospital births began in the 20th century, with the introduction of anesthesia for childbirth. However, this shift did not immediately lead to improved maternal mortality rates, and there were initially many complications and infections. It was only with the development of sulfa drugs and improved obstetric practices in the late 1930s that medical intervention during childbirth began to have a positive impact on maternal mortality.
| Characteristics | Values |
|---|---|
| Place of Birth | Before the 20th century, most women gave birth at home. |
| Medical Assistance | Midwives were the primary caregivers for women during childbirth. Male physicians trained abroad began assisting in childbirth after 1750. |
| Family and Community Involvement | Childbirth was often a community affair, with female and male relatives, attendants, and spiritual figures present. In some cultures, prayers were recited to protect the mother and ward off evil spirits. |
| Maternal Position | Women have given birth in various positions, including standing, squatting, kneeling, and sitting, as evidenced by illustrations from Ancient Egypt to recent centuries. |
| Quarantine | Some cultures practiced quarantining the mother before or after childbirth, as seen in Latin America and China. |
| Pain Management | Anesthesia existed but was not commonly used for childbirth. |
| Medical Interventions | Operative deliveries were more common in hospitals than home births. The use of forceps was introduced in the 18th century. |
| Maternal and Infant Mortality | The shift to hospital births in the early 20th century did not immediately lead to improved maternal and infant mortality rates. It was only with the development of sulfa drugs and improved obstetric practices in the late 1930s that medical intervention positively impacted mortality rates. |
| Modern Prenatal Care | The development of modern prenatal care in the last 100 years has resulted in a 99% drop in maternal death rates and a 90% decrease in childhood mortality, according to the CDC. |
What You'll Learn

Women historically gave birth at home, often with midwives
Childbirth has been a difficult process for humans throughout history. For much of human history, women gave birth at home with the help of midwives. In Tudor England (1485-1603), noblewomen would spend weeks in a "lying in" room before and after birth, receiving the blessing of a priest and the assistance of trusted midwives. In the aristocratic household of Heian Japan (794-1185), the birthing room was dressed in white and located in the north of the house.
The shift to hospital births started in the 20th century, driven by the desire for pain-free childbirth and the development of anaesthesia. However, the outcomes for women in hospitals were not always better, with high rates of complications and infections. It was not until the late 1930s, with the introduction of sulfa drugs and improved obstetric practices, that medical intervention during childbirth significantly reduced maternal mortality.
During the 1930s, most midwives practised in rural areas and were often called "granny midwives", learning their trade through their own experience. While doctors, especially obstetricians, began delivering babies in the 1940s, 50s, and 60s, the feminist movement of the 1970s revived women's interest in midwives. Today, midwives continue to assist women in childbirth, offering a happy medium between hospital and home births.
The process of childbirth has evolved, with medical pain interventions like epidurals and Doppler ultrasound technology becoming widespread. Prenatal care has also improved, with initiatives like the Ten Steps for a Mother-Friendly Childbirth focusing on the mother's wellbeing. However, in some countries where healthcare is inaccessible, death rates for mothers and babies remain high, highlighting that the process of childbirth still has room for improvement.
Safe Storage of Radioactive Isotopes in Hospitals
You may want to see also

The shift to hospital births began in the 20th century
The 20th century saw the introduction of anaesthesia for childbirth, offering women the prospect of a pain-free delivery. However, despite the promise of safer and less painful childbirth, the outcomes for women in the early 20th century were not ideal, with high rates of complications and infections. During this time, operative deliveries were much more common in hospitals than in homes, and medical experimentation and intervention were more frequent in hospital births.
In the 1930s, most midwives practised in rural areas and were often referred to as "granny midwives". The rise of hospitals and the availability of doctors, especially obstetricians, in the 1940s, 50s, and 60s, led to a decline in the use of midwives. However, the feminist movement of the 1970s revived interest in midwifery, and women began seeking alternatives like birthing centres and doulas, who provide emotional support during pregnancy and delivery.
While the shift to hospital births did not immediately lead to a decline in maternal mortality rates, the introduction of sulfa drugs and improved obstetric practices in the late 1930s positively impacted maternal survival. Over time, medical advancements, including the use of antibiotics, NICUs, and improved hygiene practices, contributed to a significant drop in maternal and childhood mortality rates.
Hospital Navigation: Door Markings in English Hospitals
You may want to see also

Medical intervention during childbirth was rare until the 1750s
For much of human history, childbirth has occurred at home, with the assistance of midwives. In many cultures, childbirth was a communal affair, with female relatives and attendants present. In some cultures, male relatives were also present. Religious figures, such as Buddhist monks, were also present to offer prayers for protection. In aristocratic households in Heian Japan (794-1185), the birthing room was dressed in white. In Tudor England (1485-1603), noblewomen were shut off in a private room for weeks before and after birth, a practice known as "lying in".
Even today, childbirth varies greatly, with some women experiencing relatively easy births and others facing extreme pain and lengthy labour. The size and shape of the modern pelvis, a result of walking upright, and the large size of a baby's head, make for a challenging birth process. While hospital births with medical intervention have become the norm in many places, some women still opt for home births with midwives or births in birthing centres.
The Impact of Straw Bans on Hospitals
You may want to see also

Maternal mortality rates did not decline with the shift to hospitals
Before the shift to hospitals, women gave birth at home, with midwives in attendance. Midwives were increasingly replaced by doctors, especially among wealthier families. Anaesthesia existed but was not commonly used for childbirth.
The shift to hospital births started in the 20th century, with the introduction of anaesthesia for delivering children. However, maternal mortality rates did not immediately decline with the move to hospitals. In the first half of the century, there were many complications and infections, and childbirth was not always safer. In the 1940s, 50s, and 60s, doctors, especially obstetricians, delivered most babies.
It was not until the discovery of antibiotics and the development of blood transfusions in the first half of the 20th century that the risk of dying in childbirth was sharply reduced. In the mid-19th century, puerperal sepsis, an infection of the uterus, was the most common cause of death in pregnancy. At the Vienna Maternity Hospital, the largest maternity hospital in the world at the time, doctors noticed a stark difference in mortality rates between the two wings of the hospital. In one wing, every tenth mother died of puerperal sepsis, while in the other, only one in 25 died. This led to the discovery that puerperal sepsis was contagious, and the importance of better hygiene and antisepsis measures was recognised. However, it was not until the second half of the 19th century that antisepsis was widely introduced into routine obstetric practice.
Today, maternal mortality rates have declined significantly, with a 99% reduction in maternal deaths over the past 100 years, according to the CDC. However, there are still large inequalities across the world, with most maternal deaths occurring in low- and lower-middle-income countries. In 2023, the maternal mortality ratio was 197 per 100,000 live births globally, and just over 90% of maternal deaths occurred in low- and lower-middle-income countries. The United States, a high-income country, has the highest rate of maternal deaths among its peers, with racial disparities contributing to the high rate.
San Ysidro Hospital Residency: Competitive Entry or Easy Access?
You may want to see also

Childbirth was a spectacle with many onlookers
Childbirth was a very different experience before the advent of hospitals as birthing centres. Women typically gave birth at home, with the aid of midwives, physicians, or other attendants. In some cases, there were no medical attendants at all, as preferred by some "freebirthers" or when the birth was unplanned.
Childbirth was often a spectacle with many onlookers. For instance, during the birth of a queen, the obstetrician announced: "The Queen is going to give birth!" and the chamber was so inundated with onlookers that the queen was nearly crushed. The crowd was described as "motley" and included two chimney sweeps who climbed onto furniture to get a better view.
The shift to hospital births started in the 20th century, driven by the desire for safer and less painful childbirth. Anesthesia was introduced for pain-free childbirth, but it did not initially provide the desired outcomes, with high rates of complications and infections. Doctors, especially obstetricians, began delivering most babies in the 1940s to 1960s, replacing midwives, who were often called "granny midwives" during this time.
The feminist movement of the 1970s revived women's interest in midwives and led to a focus on more natural types of childbirth that prioritized the mother's well-being. Today, childbirth can occur in hospitals, birth centres, or at home, with varying resources and services available depending on the setting.
Nursing Homes and Hospitals: Partners in Patient Care
You may want to see also
Frequently asked questions
Before the shift to hospital births in the 20th century, most women gave birth at home.
Women would usually be assisted by midwives, though male and female relatives and attendants would often be present as well. Wealthier families increasingly used doctors instead of midwives.
Medical intervention during childbirth has increased since the shift to hospital births. Operative deliveries, for example, were much more common in hospitals than at home. However, this shift did not lead to better outcomes, as maternal mortality rates did not decline. It was only after the development of sulfa and improved obstetric practices in the late 1930s that medical intervention decreased maternal mortality.
Childbirth was a very different experience before hospitals. In some cultures, the mother was quarantined before or after childbirth. In Tudor England, the mother would be shut off in a private room for weeks before and after birth, during which time she would receive the blessing of a priest. In aristocratic households in Heian Japan, the birthing room was dressed in white and located in the north of the house.