Testicular cancer is the most common cancer in men aged 15 to 35. It is usually first identified by a painless lump in the testicle, and it is important to get checked early as testicular cancer is highly treatable and curable. The first step is to visit a doctor, who will perform a physical examination and ask about symptoms. If they suspect testicular cancer, the next step is an ultrasound, which is a painless scan that uses high-frequency sound waves to create an image of the inside of the testicles. If the ultrasound indicates cancer, the doctor will refer the patient to a specialist, who will perform further tests, including imaging tests and blood tests, to determine the stage of the cancer and create a treatment plan.
| Characteristics | Values |
|---|---|
| Symptoms | Painless lump in the testicle, swelling or sudden fluid build-up in the scrotum, a feeling of heaviness in the scrotum, dull ache in the groin or lower abdomen, pain or discomfort in the scrotum or a testicle, shrinking testicle (testicular atrophy) |
| First Step | Physical examination by a doctor who will feel the testicles for lumps, swelling, or tenderness |
| Tests | Ultrasound, CT scans, MRI scans, blood tests, X-rays, Inguinal orchiectomy and biopsy |
| Treatment | Surgery to remove the affected testicle, chemotherapy, radiation therapy |

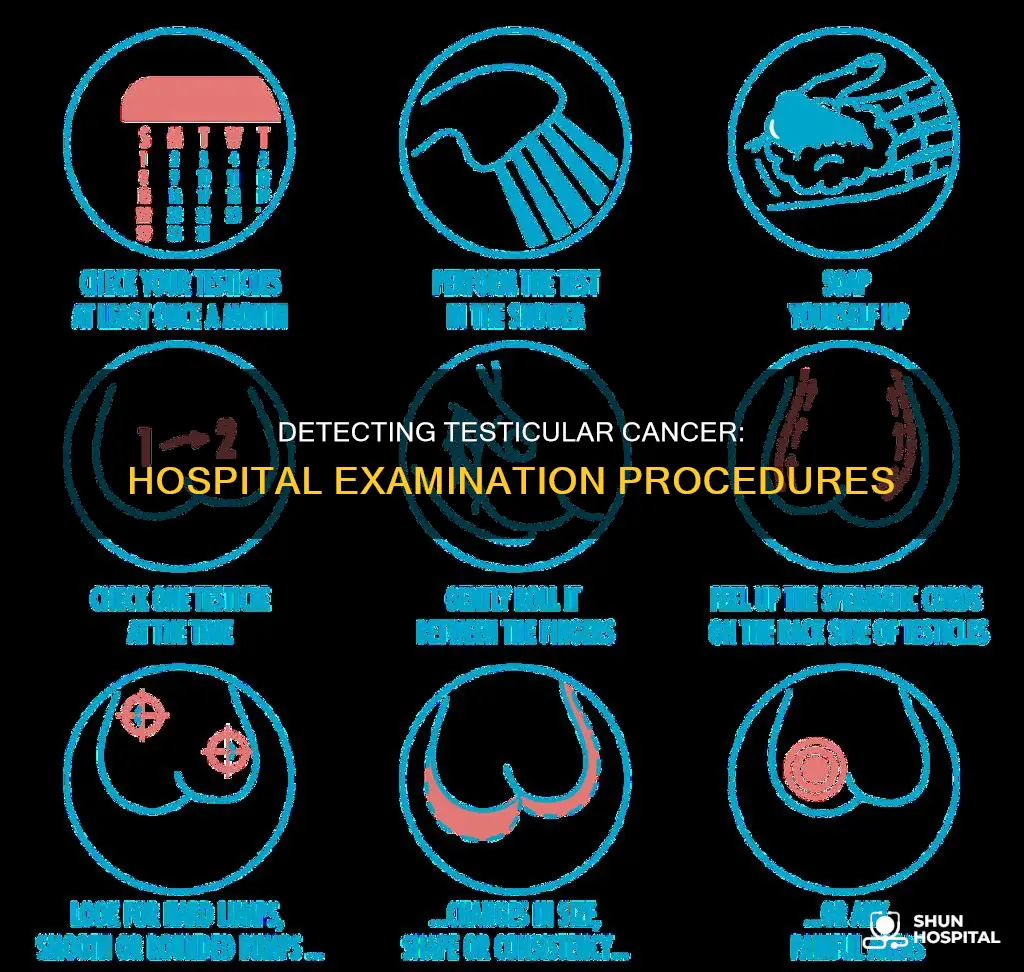
Physical examination
During a physical examination, the doctor may also listen to the patient's chest and abdomen to determine if they sound normal. If the doctor identifies any areas of concern, such as swollen or painful regions, they will pay particular attention to those areas. The results of this examination help the doctor decide whether the patient needs to be referred to a specialist for further evaluation.
One of the most common physical examination techniques used in the diagnosis of testicular cancer is the ultrasound scan. Ultrasound scans use high-frequency sound waves to create images of the internal organs. For testicular cancer, the ultrasound probe is typically placed on the patient's testicles, allowing doctors to visualise any abnormalities. Ultrasound scans are often recommended even if the doctor cannot feel a lump during the physical examination, as cancerous lumps may be too small to detect manually.
In some cases, a physical examination may also involve blood tests to check for certain proteins called tumour markers, which can be indicative of testicular cancer. These tests help doctors diagnose the condition and estimate the extent of the cancer. However, it is important to note that some cancers may be too small to elevate tumour marker levels, so negative blood test results do not always rule out the presence of cancer.
Food Poisoning: Hospital Diagnosis and Treatment Procedures
You may want to see also

Ultrasound
If the ultrasound indicates the presence of cancer, the next step is usually surgery to remove the affected testicle through an incision in the groin area. This procedure is called an orchiectomy or inguinal orchiectomy. The removed testicle is then examined under a microscope by a pathologist, who specialises in laboratory diagnosis of diseases. The pathologist sends a report describing the type and extent of the cancer, which helps in determining the appropriate treatment.
In some cases, other imaging tests may be performed before or after an ultrasound to check for the spread of cancer outside the testicles. These tests include X-rays, CT scans, and MRI scans, which can provide more detailed information about the extent and stage of the cancer.
US News Hospital Rankings: What Factors Decide?
You may want to see also

Blood tests
One such tumour marker is alpha-fetoprotein (AFP), which, when elevated, suggests the presence of a non-seminoma tumour. Non-seminoma tumours are a type of testicular cancer that arises from germ cells and tend to grow rapidly and spread beyond the testicle. However, it is important to note that some cancers may be too small to elevate tumour marker levels, so a normal AFP level does not rule out cancer.
Another tumour marker that may be evaluated in a blood test is lactate dehydrogenase (LDH). LDH is an enzyme that can be elevated in the presence of testicular cancer, indicating a widespread disease. However, it is important to interpret LDH levels with caution, as they can also be increased in some non-cancerous conditions.
Overall, blood tests are an essential tool in the diagnosis and management of testicular cancer. They help doctors identify tumour markers, such as AFP and LDH, which can indicate the presence and extent of the disease. By combining blood tests with other diagnostic techniques, healthcare professionals can make informed decisions about treatment options and improve patient outcomes.
The Hospital Where Martin Luther King Died
You may want to see also

Imaging tests
Ultrasounds are not the only imaging tests used to diagnose testicular cancer. If cancer is detected, doctors will often order additional imaging tests to determine if it has spread to other parts of the body. These tests may include X-rays, CT scans, and MRI scans. X-rays can be used to image the chest and determine if cancer has spread to the lungs. CT scans, which use X-rays and computers to create detailed 3D images, can show if the cancer has spread to the lymph nodes, lungs, liver, or other organs. MRI scans, meanwhile, are particularly useful for examining the brain and spinal cord.
Together, these imaging tests help doctors understand the stage of the cancer, which informs treatment recommendations. Testicular cancer is typically divided into four stages based on its spread. Stage 1 indicates that the cancer is contained within the testicle, while Stages 2 and 3 involve spread to the lymph nodes and other areas of the body, respectively. Stage 4 indicates that the cancer has metastasised or spread widely throughout the body.
While imaging tests are essential for diagnosing and staging testicular cancer, they are just one component of the diagnostic process. Doctors also rely on physical examinations, blood tests, and, in some cases, surgery to confirm the presence of cancer and guide treatment decisions.
Hospitals' Battle Plan Against COVID-19
You may want to see also

Orchiectomy and biopsy
Orchiectomy is a surgical procedure to remove one or both testicles. It is a common treatment option for testicular cancer. The surgery can be used as a diagnostic tool, as well as to prevent and treat the disease. During an orchiectomy, an incision is made in the patient's groin (inguinal orchiectomy) or scrotum (simple orchiectomy). If the whole testicle is removed, the procedure is known as a radical orchiectomy. When only the tumour and a margin of healthy tissue are removed, it is called a partial orchiectomy. Orchiectomies are typically performed as outpatient procedures, meaning the patient can go home on the same day.
After an orchiectomy, a pathologist examines the tissue removed from the patient's testicle under a microscope to check for cancer cells. This process is known as a biopsy. The pathologist's report will determine the treatment the patient receives. The biopsy allows the pathologist to determine what stage of testicular cancer the patient has, if any. Staging is the process of finding out how far the cancer has spread, which is crucial as treatment options and prognosis depend on the "stage" of cancer.
If the orchiectomy and biopsy confirm testicular cancer, the patient may undergo chemotherapy or radiation therapy to destroy any remaining cancer cells or prevent the cancer from returning. When treating advanced-stage testicular cancer that has spread, chemotherapy may be given before an orchiectomy.
Not everyone who has an orchiectomy chooses to get a testicular implant. However, for those who do, it may alleviate concerns about their appearance and increase their confidence.
Chang Gung Memorial Hospital: A Comprehensive Healthcare Giant
You may want to see also
Frequently asked questions
Hospitals use a variety of tests to check for testicular cancer. The first step is usually a physical examination by a doctor, who will feel the testicles for lumps, swelling, or tenderness. They will also examine other parts of the body, such as the abdomen, lymph nodes, and chest, for signs of cancer spread. If a lump or other symptoms are found, further testing is often required, including:
- Ultrasound: A painless scan that uses sound waves to create images of the inside of the testicles.
- Blood tests: To check for tumor markers, such as AFP and LDH, which can indicate the presence of cancer.
- Imaging tests: If cancer is detected, imaging tests such as X-rays, CT scans, and MRI scans may be used to determine the extent of cancer spread.
- Orchiectomy and biopsy: If the ultrasound indicates cancer, the affected testicle is removed through an incision in the groin, and a pathologist examines the tissue for cancer cells under a microscope.
The most common sign of testicular cancer is a painless lump in one or both testicles. Other symptoms include swelling or fluid build-up in the scrotum, a feeling of heaviness in the scrotum, a dull ache in the groin or lower abdomen, pain or discomfort in the scrotum or testicle, and shrinking of the testicle (testicular atrophy). It is important to note that these symptoms can also be caused by other conditions, so a proper diagnosis by a medical professional is necessary.
Testicular cancer arises from germ cells in the testicles, which can form a mass or tumor. There are two main types of testicular cancer:
- Seminoma: This is a slow-growing type of cancer that usually affects people in their 40s or 50s. It is typically limited to the testicle but can occasionally spread to other parts of the body.
- Non-seminoma: This type of cancer grows more rapidly and is more likely to spread beyond the testicle. It mainly affects younger individuals in their late teens to early 30s. There are four types of non-seminoma tumors: embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma.