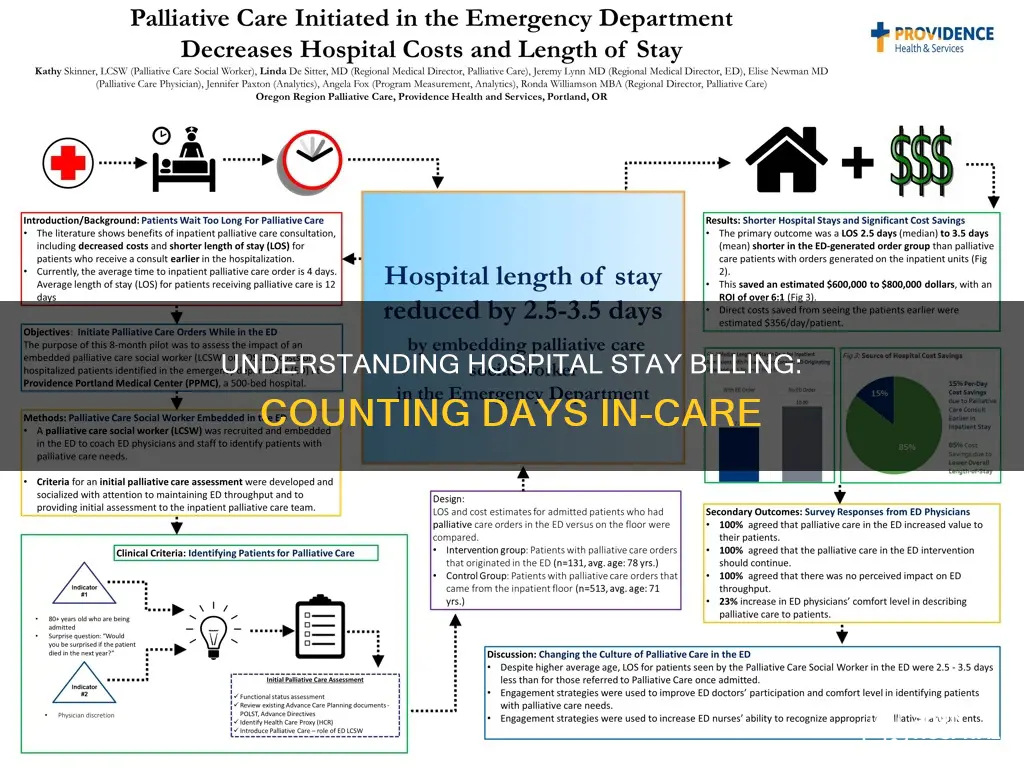
Hospitals use various methods to calculate a patient's length of stay (LOS), which is the duration of a single hospitalisation episode. The counting method depends on the research question and the type of analysis being conducted. The most common methods include using the original LOS for each separation within a year, truncating the LOS at 365 days, or counting only the in-year days. The average length of stay (ALOS) is a common statistic calculated by dividing the sum of inpatient days by the number of patient admissions with the same diagnosis-related group classification. LOS is often used as a quality metric, with shorter stays promoted by payment systems, and is linked to other quality indicators such as patient satisfaction and readmission rates.
| Characteristics | Values |
|---|---|
| Counting Method | Depends on the research question, i.e., costing analysis, diagnosis/procedure-specific, or population-based |
| Length of Stay (LOS) | Variable denoting the number of days an individual spent in the hospital |
| Total Length of Stay | Refers to the rates and other day count measures |
| Average Length of Stay (ALOS) | Calculated by dividing the sum of inpatient days by the number of patient admissions with the same diagnosis-related group classification |
| In-Year Days | Used for small area analysis/institutional analysis to avoid the impact of very long stays on small institutions |
| LOS "Over Time" Definition | Counts the days that are part of the fiscal year of discharge |
| LOS Truncated at 365 Days | Method used in some MCHP research, truncating all LOS greater than 365 at 365 days |
| Quality Metric | Length of stay is linked to quality metrics such as patient satisfaction, reduction in hospital readmissions, and mortality |
What You'll Learn
- Counting methods depend on research questions, e.g. costing analysis, diagnosis/procedure-specific or population-based
- Length of Stay (LOS) is the variable denoting the number of days spent in hospital
- LOS can be calculated by subtracting the day of admission from the day of discharge
- The average length of stay (ALOS) is a mean calculated by dividing the sum of inpatient days by admissions
- Regression models and Markov chain methods are used to model length of stay in different condition contexts

Counting methods depend on research questions, e.g. costing analysis, diagnosis/procedure-specific or population-based
The counting method used to determine hospital days or length of stay (LOS) depends on the nature of the research question. For instance, whether the research is focused on costing analysis, diagnosis/procedure-specific analysis, or population-based analysis.
When it comes to costing analysis, the perspective of the analysis is crucial. This often implies considering the costs borne or paid by the budget of the decision-maker's organisation. For example, in the context of healthcare providers, full absorption costing may be employed, where direct, variable, and fixed overhead costs are allocated to all cost objects. Fixed overhead costs can include items like amortisation of buildings, interest payments, insurance, staff training, and general administration. However, the inclusion of these fixed costs in economic evaluations will depend on the specific research question and context.
In diagnosis/procedure-specific analysis, the counting method may depend on the specific condition or procedure being studied. For instance, in research on medical imaging for diagnoses, the choice of imaging modality (such as CT, MRI, X-ray, or ultrasound) depends on the disease, organ, and specific clinical questions being addressed.
Population-based analysis, on the other hand, involves studying a defined and relatively heterogeneous population of patients over time. This can include a country, a specific geographical area, an insured population, or a clinic population. Cross-sectional cost-of-illness studies, also known as prevalence-based studies, provide insights into utilisation and cost relationships within a defined population. On the other hand, longitudinal cost-of-illness studies, or incidence-based studies, focus on the cost of caring for an individual or a homogenous group of individuals over a specific period.
Additionally, when comparing data from different jurisdictions or previous analyses, it is important to specify the usual way of measuring days, as methods can vary. For instance, the "Over Time" definition counts the days that are part of the fiscal year of discharge. This method was used by Roos et al. in 2001, where they checked if the admission date was before April 1, 1998, for all hospital claims in the 98/99 dataset.
Roseburg VA Hospital: Size and Scope
You may want to see also

Length of Stay (LOS) is the variable denoting the number of days spent in hospital
Various methods have been used to count hospital days, depending on the nature of the research question. For example, when conducting small area analysis or institutional analysis, using in-year days is recommended to avoid the impact of very long stays on small institutions. This method only considers hospital days that fall within the fiscal year. Another approach is to use the original LOS for each separation within the year, although this may overcount in small areas due to extended stays in some hospitals.
To address this issue, a third method involves truncating the original LOS at 365 days for each separation falling within the year. This approach ensures that extremely long stays do not skew the data. The specific method chosen for measuring LOS should be dated and clearly specified, as different counting methods can be employed depending on the context and research objectives.
LOS is often used as a quality metric, with shorter stays being promoted by payment systems to incentivize hospitals to provide efficient care. Additionally, LOS can be linked to other quality indicators such as patient satisfaction, readmission rates, and mortality. Discharge planning processes can play a role in reducing a patient's LOS, and predicting or modelling LOS can help identify factors influencing hospital stays.
Hospital Ships: Giant Navy Vessels Saving Lives
You may want to see also

LOS can be calculated by subtracting the day of admission from the day of discharge
The length of stay (LOS) in a hospital is a measure of the duration of a single episode of hospitalisation. LOS is calculated by subtracting the day of admission from the day of discharge. This calculation gives the number of inpatient days for an individual.
The average length of stay (ALOS) is a separate concept and is a mean calculated by dividing the sum of inpatient days by the number of patient admissions with the same diagnosis-related group classification. ALOS can also be calculated by considering only the length of stay during the period under analysis. It is important to distinguish between LOS and ALOS, as well as "hospital days" or simply "days".
Various methods have been used to count hospital days, depending on the research question and context. For example, when performing small area analysis or institutional analysis, using in-year days can prevent very long stays from affecting days in small institutions. Another method is to truncate the original LOS at 365 days for each separation falling within the year.
The LOS can also be calculated differently when considering only part of a fiscal year, as demonstrated by Roos et al. (2001). In their method, for hospital claims on the 98/99 dataset, the admission date was checked against April 1, 1998. If the admission date was before April 1, 1998, the LOS was re-calculated as the separation date minus April 1, 1998. This approach ensures that stays spanning multiple years are accurately counted within the respective fiscal years.
Jackson Avery: The Downfall of Seattle Grace Hospital
You may want to see also

The average length of stay (ALOS) is a mean calculated by dividing the sum of inpatient days by admissions
The average length of stay (ALOS) in a hospital is a statistical measure that helps administrators and researchers understand the duration of a typical hospitalisation. It is calculated by taking the sum of inpatient days and dividing it by the number of admissions, providing a mean value. This calculation can be adjusted to include only patients with the same diagnosis-related group classification, ensuring more accurate comparisons.
ALOS is an important metric for hospitals as it provides insights into the efficiency of care delivery and resource utilisation. By understanding the average duration of hospital stays, administrators can make informed decisions about staffing, bed occupancy, and resource allocation. It also serves as a quality indicator, with shorter lengths of stay potentially indicating effective discharge planning or improved patient outcomes.
The calculation of ALOS can vary depending on the specific research question or analysis being conducted. For instance, in small area or institutional analyses, using in-year days can prevent the distortion caused by very long stays in small hospitals. This involves considering only the hospital days falling within a specific fiscal year, ensuring that extended stays do not disproportionately impact the average.
Additionally, different methods have been employed to address the issue of very long stays. One approach is to use the original length of stay for each separation within a year, although this may result in overcounting in small areas. Another method involves truncating the original length of stay at 365 days for each separation, ensuring that extremely long stays do not skew the average.
It is worth noting that while ALOS provides a useful mean value, it may not accurately represent a typical length of stay due to the highly skewed nature of hospitalisation durations. In such cases, the median may be a preferred measure. Furthermore, predictive models and statistical approaches, such as regression models or Markov chain methods, can be utilised to analyse and predict factors influencing length of stay, allowing hospitals to optimise their practices and improve patient care.
Abortion Procedures: What to Expect in the Hospital
You may want to see also

Regression models and Markov chain methods are used to model length of stay in different condition contexts
Hospitals use different methods to count the days of a patient's stay, depending on the context and purpose of the analysis. The variable that denotes the number of days a patient spends in the hospital is called Length of Stay (LOS).
When it comes to modelling length of stay in different condition contexts, regression models and Markov chain methods can be used. Regression models are statistical techniques that examine the relationship between variables to make predictions. On the other hand, Markov chains are used to model a sequence of events where the probability of the next event depends only on the current state of the process, not on previous states. This is known as the Markov Property.
Markov models are structured around health states and movements between them. In a healthcare context, a patient's health can be split into distinct categories or health states, such as "well", "disease", and "dead". The patient can only occupy one state at a time and will remain in that state for a specified period. At the end of each cycle, the patient can either stay in the same state or move to another health state. Markov models can be used to predict the length of time patients will stay in each state and the associated costs and outcomes.
Markov chain methods have been applied in various healthcare contexts, including disease outbreak and epidemic modelling, automatic speech recognition systems, and web navigation behaviour analysis. They are also used for forecasting in several areas, such as price trends and wind power. Regression models, on the other hand, can be used to identify factors that influence length of stay and make predictions about future stays based on those factors.
Women's Influence on Hospitality: A Powerful Force
You may want to see also
Frequently asked questions
The number of days a patient has stayed in the hospital is calculated by subtracting the day of admission from the day of discharge.
LOS stands for Length of Stay, which is the duration of a single episode of hospitalization. ALOS stands for Average Length of Stay, which is the mean calculated by dividing the sum of inpatient days by the number of patient admissions with the same diagnosis-related group classification.
The counting method used by hospitals depends on the purpose of the research. For example, when conducting a costing analysis, it is recommended to use allocated in-year days. If the research is diagnosis/procedure-specific or population-based, other methods may be more suitable.