Hospitals employ various methods to drain fluid from the lungs, including thoracentesis, thoracoscopy, and chest tube insertion. Thoracentesis is a common procedure involving the insertion of a needle and catheter to drain excess fluid from the pleural space, the area between the lungs and chest wall. It is often performed as an outpatient procedure with local anesthesia, taking around 15 minutes. Thoracoscopy, on the other hand, is a minor surgical operation performed in an endoscopy suite or operating theater. Chest tube insertion can be done at the end of a surgical procedure or at the bedside, and the tubes are typically connected to drainage systems. These procedures help alleviate chest pressure, improve lung function, and aid in diagnosing underlying health issues.
| Characteristics | Values |
|---|---|
| Procedure | Thoracentesis, thoracocentesis, pleural aspiration, pleural tap, chest tap, thoracoscopy, laparoscopy, chest tube procedure |
| Purpose | Drain excess fluid from the lungs, diagnose health problems, check for cancer cells |
| Fluid Drained From | Space between the lungs and the wall of the chest (pleural cavity) |
| Position | Sitting on a chair or bed with arms resting on a table |
| Anaesthesia | Local anaesthesia |
| Instruments | Needle, catheter (tube) |
| Duration | 15 minutes |
| Recovery | Avoid strenuous activity for a few days, resume normal activities when able |
| Risks | Air in the pleural space (pneumothorax), infection, bleeding |
What You'll Learn
- Thoracentesis: a nonsurgical procedure to drain fluid from the pleural cavity
- Pleural effusion: a condition caused by excess fluid in the pleural cavity, requiring thoracentesis
- Pleural tap: another term for thoracentesis, a procedure to drain fluid from the pleural space
- Chest tubes: plastic tubes inserted to drain fluid or air from the chest cavity
- Thoracoscopy: a small operation to drain fluid from the lungs or abdomen

Thoracentesis: a nonsurgical procedure to drain fluid from the pleural cavity
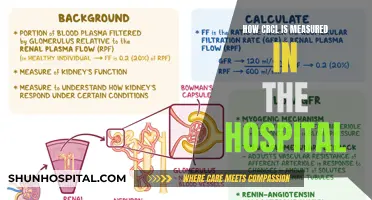
Thoracentesis is a nonsurgical procedure used to drain excess fluid from the pleural cavity, the space between the lungs and the chest wall. This fluid buildup is known as pleural effusion and can be caused by various medical conditions, including cancer, congestive heart failure, and infections such as tuberculosis. Pleural effusion puts pressure on the lungs, making it difficult to breathe.
During the procedure, patients are typically awake and asked to sit on a chair or bed, leaning forward with their arms resting on a table. This position widens the spaces between the ribs, making it easier for the doctor to access the pleural cavity. The doctor will then clean and numb the area with a local anesthetic. A thin, hollow needle is inserted between the ribs, through the chest wall, and into the pleural cavity. A catheter (tube) may also be attached to the needle to aid in withdrawing the fluid. Ultrasound imaging is often used to guide the needle insertion and ensure accuracy.
Thoracentesis is usually a brief procedure, lasting about 15 minutes, although it may take longer if there is a significant amount of fluid to remove. After the procedure, the needle is removed, and the area is bandaged. Patients may cough for up to an hour afterward as their lungs re-expand. It is common to experience some discomfort and pressure during the procedure, and patients may feel groggy from the medication. Following the procedure, it is recommended to avoid strenuous activity for a few days, and patients can resume normal daily activities as they feel able.
In addition to providing relief from excess fluid, thoracentesis also serves a diagnostic purpose. The drained fluid is sent to a laboratory for testing to determine the underlying cause of the buildup. Conditions such as congestive heart failure, infections, and cancer can be detected through this process. Therefore, thoracentesis plays a crucial role in both the treatment and diagnosis of pleural effusions.
Hospitals: How Close is Too Close?
You may want to see also

Pleural effusion: a condition caused by excess fluid in the pleural cavity, requiring thoracentesis
Pleural effusion is a condition caused by excess fluid in the pleural cavity, which is the space between the lungs and the wall of the chest. Normally, this space contains only a small amount of fluid that lubricates the membranes surrounding the lungs, but certain health conditions can cause a buildup of fluid, leading to pleural effusion. This excess fluid puts pressure on the lungs and makes it difficult to breathe.
Hospitals use a procedure called thoracentesis to drain fluid from the lungs in cases of pleural effusion. Thoracentesis involves inserting a needle through the skin of the chest into the pleural cavity to remove the excess fluid. This procedure is typically done on an outpatient basis and usually takes about 15 minutes. However, it may take longer if there is a large amount of fluid to remove.
During thoracentesis, the patient is positioned on the edge of a chair or bed with their head and arms resting on an examination table. The doctor will then sterilize and numb the area where the needle will be inserted. The doctor will insert the needle between the ribs on the patient's back and into the pleural cavity. A catheter (a small tube) may also be attached to the needle to help withdraw the fluid.
Thoracentesis is a minimally invasive procedure that carries a low risk of complications when performed with the appropriate technique and precautions. It is used for both diagnostic and therapeutic purposes, as it helps alleviate symptoms of pleural effusion and provides crucial information about the underlying cause of the fluid buildup. After the procedure, the patient may experience some discomfort, such as coughing or a burning sensation, as their lungs re-expand.
Hospitals' Strategies to Combat Acquired Infections
You may want to see also

Pleural tap: another term for thoracentesis, a procedure to drain fluid from the pleural space
Thoracentesis, also known as pleural tap, thoracocentesis, or pleural aspiration, is a procedure to drain excess fluid from the pleural space, the area between the lungs and the chest wall. This procedure is typically performed in a hospital setting and can last anywhere from 15 minutes to an hour.
During the procedure, patients are usually awake and asked to remove their upper body clothing and put on a hospital gown. A comfortable sitting position is recommended, with the arms resting on a table to spread out the space between the ribs. The medical team will then clean and numb the area on the patient's back where the procedure will take place.
A small cut is made, and a needle attached to a catheter (tube) is inserted through the cut and into the pleural space. Ultrasound imaging is often used to guide the needle accurately into the pleural space. The excess fluid is then drained through the catheter into a container. Once enough fluid has been drained, the needle is removed, and a small dressing is applied to the area.
The drained fluid is then sent to a laboratory for testing to determine the cause of the fluid buildup. This can include testing for infections, illnesses, or other causes of pleural effusion. The procedure helps relieve chest pressure and improves breathing by reducing the excess fluid in the pleural space.
China's Healthcare System: Hospitals' Business Organization
You may want to see also

Chest tubes: plastic tubes inserted to drain fluid or air from the chest cavity
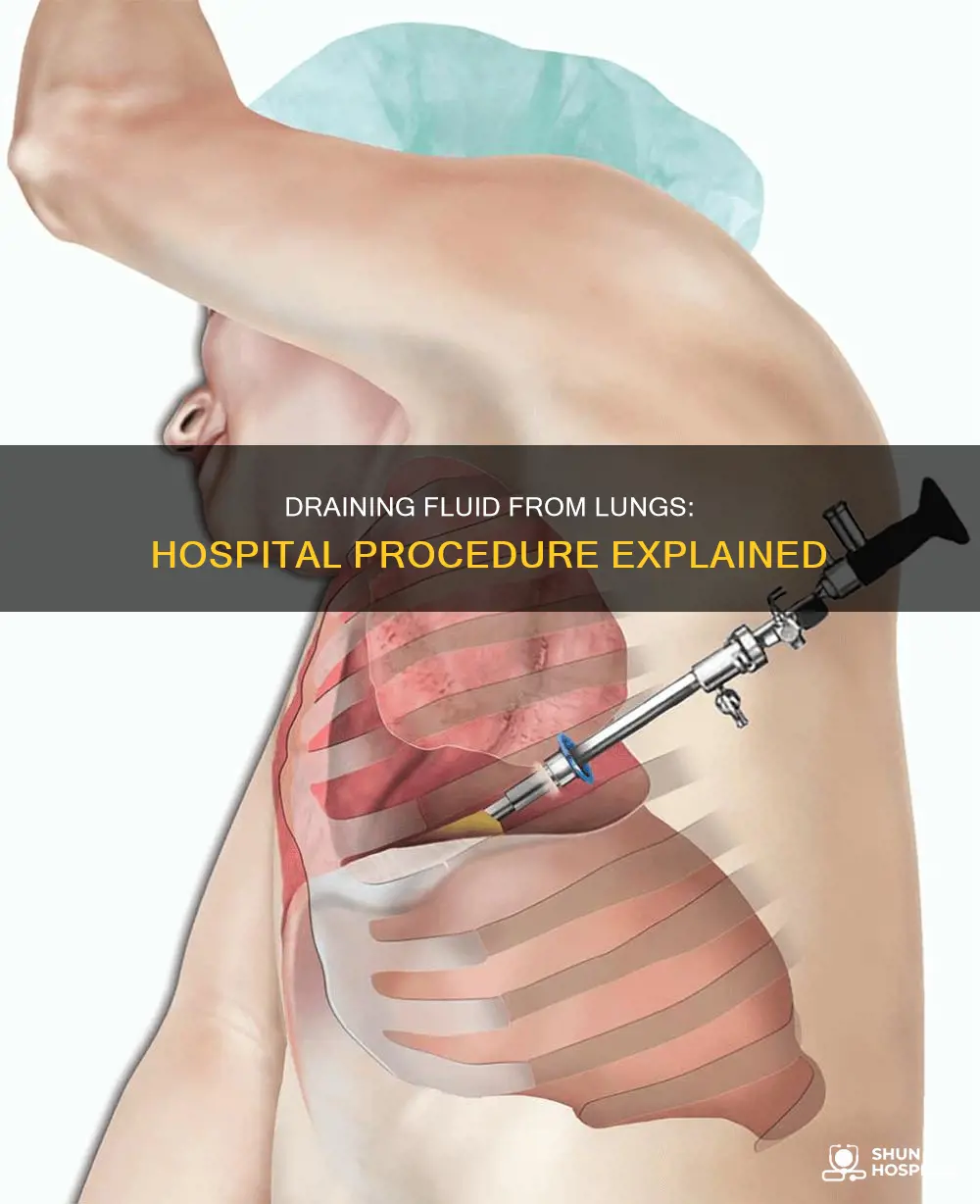
A chest tube, also known as a thoracostomy tube, is a medical device used to drain fluid or air from the chest cavity, specifically the pleural space—the region between the lungs and chest wall. These plastic tubes come in various shapes and sizes, ranging from as small as a shoelace to as large as a highlighter in diameter. They are usually connected to drainage systems that collect fluid and allow air to escape from the chest.
Chest tubes are typically inserted while a patient is asleep from anesthesia following a surgical procedure or at the bedside using local pain killers and sedation. The tubes are placed in a well-defined anatomical region known as the safe triangle, which minimizes the risk of complications during insertion. This region is bordered anteriorly by the pectoralis major, posteriorly by the latissimus dorsi, and inferiorly by a horizontal line at the nipple level.
The insertion process may involve cutting and gently spreading the skin and muscles of the chest wall or inserting a wire through a needle to guide the tube. Patients commonly experience discomfort during and after the procedure, but pain medications can help manage this. Mild discomfort is expected as the tube lies on the ribs and moves with each breath.
Chest tubes remain in place for several days, depending on the amount of fluid being drained and the presence of air escaping. They are typically removed when drainage is low or there is no more air escaping. Proper placement, secure connections, and continuous monitoring are crucial to prevent complications such as infection, dislodgment, or tube occlusion.
Testing Strategies for the Delta Variant: A Hospital Guide
You may want to see also

Thoracoscopy: a small operation to drain fluid from the lungs or abdomen
Thoracoscopy is a small operation to drain fluid from the lungs or abdomen. It is often carried out as a day procedure, but patients may need to stay in hospital overnight.
The patient is given a local anaesthetic and remains awake during the procedure. To drain fluid from the lungs, the patient sits on a chair or the edge of a bed, leaning forward over a table with a pillow on it. For fluid in the abdomen, the patient can lie down on a bed or a reclining chair. The doctor will then insert a needle (cannular) into the chest or abdomen to drain the fluid. This is often guided by ultrasound or chest X-ray imaging.
Thoracoscopy is a relatively safe procedure, but there are some risks, including the tube blocking, air collecting in the pleural space (pneumothorax), infection, and bleeding. Patients may experience some pain and discomfort during and after the procedure, which can be managed with pain medication.
Following the procedure, the patient's blood pressure, pulse, and breathing will be closely monitored. They may cough for up to an hour afterward as their lungs re-expand. The drained fluid will be sent to a lab for testing to determine the cause of the fluid buildup.
Urine Drug Tests: Accuracy in Medical Settings
You may want to see also
Frequently asked questions
Hospitals drain fluid from the lungs through a procedure called thoracentesis, which involves inserting a thin, hollow needle between the ribs, through the chest wall and into the pleural cavity.
Thoracentesis is performed to drain excess fluid from the pleural cavity, also known as the pleural space, which is the space between the lungs and the chest wall. This excess fluid can cause difficulty in breathing and chest pressure.
During thoracentesis, patients are typically awake and given a local anesthetic to numb the area. The doctor will insert a needle between the ribs in the back, often guided by ultrasound imagery, and attach a catheter (tube) to drain the fluid. The procedure usually takes about 15 minutes, and patients may cough for up to an hour afterward as the lungs re-expand.