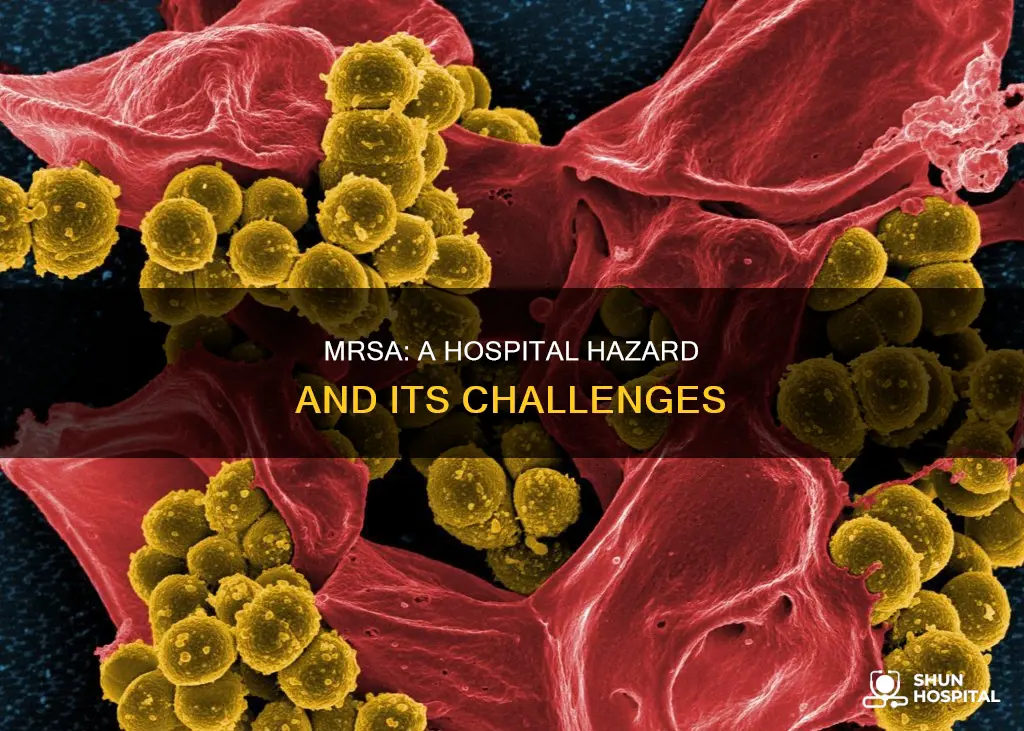
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of staph bacteria that is resistant to many antibiotics used to treat ordinary staph infections. MRSA infections often occur in healthcare settings such as hospitals, nursing homes, and dialysis centers, and they can be life-threatening. The bacteria usually enter the body through a cut or wound, causing skin problems and potentially serious infections in the bones, joints, heart valves, lungs, and bloodstream. MRSA is commonly spread through touch, including via healthcare workers with unclean hands or contaminated surfaces. According to estimates, approximately 3.2 million patients admitted to hospitals in the European Union acquire healthcare-associated infections each year, with MRSA being the predominant cause.
| Characteristics | Values |
|---|---|
| How it spreads | Through touch, contaminated hands, invasive devices such as catheters, or surgery. |
| Where it spreads | Hospitals, nursing homes, dialysis centres, and other healthcare settings. |
| Risk factors | Long hospital stays, serious conditions, breaks in the skin, cuts, wounds, burns, etc. |
| Symptoms | Red bumps, boils, abscesses, skin infections, pneumonia, bone infections, endocarditis, etc. |
| Treatment | Antibiotics, surgical draining, special nasal cream or spray, body wash, and shampoo. |
| Prevention | Cleaning, hand hygiene, infection control training, appropriate antibiotic prescribing, etc. |
What You'll Learn
- MRSA is caused by antibiotic resistance, which is linked to unnecessary antibiotic use
- MRSA is spread through touch, contaminated surfaces, and invasive devices
- MRSA can cause serious infections, including in bones, joints, the heart, and lungs
- MRSA is more prevalent in hospitals due to factors like poor cleaning and hand hygiene.
- MRSA can be treated with antibiotics, but some strains are resistant to certain antibiotics

MRSA is caused by antibiotic resistance, which is linked to unnecessary antibiotic use
MRSA (Methicillin-resistant Staphylococcus aureus) is a type of staph bacteria that has become resistant to many of the antibiotics used to treat ordinary staph infections. MRSA is the result of decades of often unnecessary antibiotic use. For years, antibiotics have been prescribed for colds, flu, and other viral infections that do not respond to these drugs. Even when antibiotics are used appropriately, they contribute to the rise of drug-resistant bacteria because they do not destroy every germ they target. Bacteria live on an evolutionary fast track, so germs that survive treatment with one antibiotic soon learn to resist others.
MRSA infections often occur in healthcare settings, such as hospitals, nursing homes, and dialysis centers. When it occurs in these settings, it is known as health care-associated MRSA (HA-MRSA). HA-MRSA can spread through healthcare workers touching patients with unclean hands or patients touching unclean surfaces. It is also associated with invasive procedures or devices, such as surgeries, intravenous tubing, or artificial joints.
In hospitals, MRSA can cause serious problems as it can lead to bloodstream infections and other life-threatening infections in bones, joints, surgical wounds, the heart, lungs, spleen, kidney, or spine. It can also cause abscesses that require surgical draining.
To prevent and control MRSA infections in hospitals, it is crucial to improve cleaning standards, hand hygiene, and infection control training. Additionally, appropriate antibiotic prescribing practices are essential to reducing the development of antibiotic-resistant bacteria, including MRSA.
Hospitals: Securing Data Backups for Patient Care
You may want to see also

MRSA is spread through touch, contaminated surfaces, and invasive devices
MRSA, or Methicillin-resistant Staphylococcus aureus, is a type of staph bacteria that has become resistant to many of the antibiotics used to treat ordinary staph infections. MRSA usually lives harmlessly on the skin and spreads through touch. It can spread when someone with MRSA on their skin touches another person or an object, and then someone else touches that object.
MRSA can also spread through contaminated surfaces. This can happen when healthcare workers touch patients with unclean hands or when patients touch unclean surfaces. Poor hand hygiene and insufficient cleaning staff in hospitals have been identified as factors contributing to the spread of MRSA.
Invasive devices, such as surgeries, intravenous tubing, artificial joints, and catheters, are another way MRSA can spread in hospitals. These devices can become contaminated and introduce MRSA bacteria into the body, causing serious infections.
While MRSA can cause minor skin problems, it can also burrow deep into the body and cause potentially life-threatening infections in bones, joints, surgical wounds, the bloodstream, heart valves, lungs, spleen, kidney, or spine. It is important to seek medical attention if wounds appear infected or are accompanied by a fever.
Childhood Trauma: Hospital Procedures' Lasting Impact
You may want to see also

MRSA can cause serious infections, including in bones, joints, the heart, and lungs
MRSA (methicillin-resistant Staphylococcus aureus) is a type of staph bacteria that has become resistant to many antibiotics used to treat ordinary staph infections. MRSA infections frequently occur in healthcare settings, but they can also happen anywhere. MRSA can cause serious illnesses that are challenging to treat due to antibiotic resistance.
MRSA can cause potentially life-threatening infections in bones, joints, the heart, and lungs. Staph skin infections, including MRSA, often begin as swollen, painful red bumps resembling pimples or spider bites. These bumps can rapidly develop into deep, painful boils (abscesses) requiring surgical drainage. While sometimes the bacteria remain confined to the skin, they can also penetrate deeper into the body, leading to severe infections.
Infections in bones and joints can result from MRSA entering the body through cuts or wounds. These infections can be life-threatening and may require surgical intervention. Additionally, MRSA can cause infections in the heart valves, leading to serious complications such as sepsis, septic shock, and respiratory failure.
MRSA can also cause respiratory issues and infections in the lungs. The bacteria can spread to the lungs through the bloodstream or by entering the body through cuts or wounds. Pneumonia and other respiratory infections may develop, which can be particularly dangerous for individuals with underlying lung conditions or compromised immune systems.
The impact of MRSA on bones, joints, the heart, and lungs underscores the importance of early detection and effective treatment. While MRSA infections can be challenging to manage due to antibiotic resistance, prompt medical attention and appropriate wound care are crucial to preventing severe complications and reducing the risk of life-threatening situations.
China's Healthcare System: Hospitals' Business Organization
You may want to see also

MRSA is more prevalent in hospitals due to factors like poor cleaning and hand hygiene.
MRSA (Methicillin-resistant Staphylococcus aureus) is a type of bacteria that usually lives harmlessly on the skin. However, if it gets inside the body, it can cause serious infections that require immediate treatment with antibiotics. MRSA infections often occur in healthcare settings, with most cases occurring in individuals who have been hospitalized or in other healthcare settings like nursing homes and dialysis centres. When MRSA is contracted in these settings, it is known as healthcare-associated MRSA (HA-MRSA).
HA-MRSA infections are typically associated with invasive procedures or devices, such as surgeries, intravenous tubing, or artificial joints. The spread of HA-MRSA can occur through healthcare workers with unclean hands or when patients touch unclean surfaces. Poor cleaning practices and inadequate hand hygiene standards in hospitals have been identified as significant contributors to the prevalence of MRSA infections. Studies have shown a decrease in MRSA incidents with improved general cleaning and hand hygiene practices.
In addition to poor cleaning and hand hygiene, insufficient infection control training among healthcare staff can also increase the risk of MRSA transmission. Creating a favourable error-reporting climate is essential to addressing these issues. By encouraging a culture where employees feel comfortable reporting and discussing errors, near misses, and incidents, hospitals can better identify and learn from system failures and implement effective measures to reduce MRSA infections.
Furthermore, inappropriate antibiotic prescribing practices have been linked to the development of MRSA infections. Antibiotic resistance is a significant problem, and the indiscriminate use of antibiotics contributes to the emergence of drug-resistant bacteria like MRSA. Up to 50% of antibiotics may be unnecessary or improperly prescribed, leading to the killing of beneficial bacteria that protect the body from infection. This allows antibiotic-resistant bacteria to multiply and cause infections, including MRSA.
MRSA infections can cause various health issues, including skin infections, pneumonia, bone infections, and endocarditis (heart valve infections). These infections can become life-threatening if the bacteria spread to the bones, joints, surgical wounds, bloodstream, heart valves, or lungs. Therefore, addressing the factors contributing to the prevalence of MRSA in hospitals, such as poor cleaning, inadequate hand hygiene, insufficient infection control training, and inappropriate antibiotic use, is crucial to preventing and managing this challenging healthcare issue.
Strict Visiting Hours: How Hospitals Keep Order
You may want to see also

MRSA can be treated with antibiotics, but some strains are resistant to certain antibiotics
MRSA (Methicillin-Resistant Staphylococcus Aureus) is a type of bacteria that is resistant to several antibiotics. It is a common cause of hospital-acquired infections and can affect anyone, but the risk is higher for people with frequent hospitalizations, skin-to-skin contact with others, and exposure to crowded and unhygienic places.
MRSA infections can cause a wide range of symptoms depending on the affected part of the body. They often occur in healthcare settings and are associated with invasive procedures or devices, such as surgeries, intravenous tubing, or artificial joints. The bacteria can cause skin infections, pneumonia, bone infections, and endocarditis (heart valve infections), among other issues.
While MRSA can be treated with antibiotics, some strains have developed resistance to certain antibiotics. For example, MRSA is resistant to methicillin, nafcillin, cephalosporin, and penicillin. However, it can usually be treated with vancomycin, an antibiotic administered through an IV. Unfortunately, some strains of MRSA have also developed some resistance to vancomycin, making them more challenging to treat.
The distinction between community-associated MRSA (CA-MRSA) and healthcare-associated MRSA (HA-MRSA) is essential in understanding antibiotic resistance. CA-MRSA infections occur in healthy people outside of healthcare settings, while HA-MRSA is associated with hospitals and other healthcare environments. HA-MRSA has a higher resistance to antibiotics than CA-MRSA, and specific antibiotics may be more effective for treating one type over the other.
The development of antibiotic resistance in MRSA is a significant concern. It is believed to be the result of decades of unnecessary antibiotic use and even appropriate antibiotic use. As bacteria evolve rapidly, germs that survive treatment with one antibiotic can quickly become resistant to others. To address this challenge, newer antibiotics are being developed, and careful hand washing remains the most effective way to control the spread of MRSA.
Promoting Equality: Healthcare's Diversity Commitment
You may want to see also
Frequently asked questions
MRSA stands for Methicillin-resistant Staphylococcus aureus. It is a type of bacteria that usually lives harmlessly on the skin but can cause serious infection if it gets inside the body.
MRSA infections often occur in healthcare settings, such as hospitals, nursing homes, and dialysis centers. They are usually associated with invasive procedures or devices, such as surgeries, intravenous tubing, or artificial joints. MRSA can spread through touch, such as healthcare workers touching patients with unclean hands or patients touching unclean surfaces.
Staph skin infections, including MRSA, usually start as swollen, painful red bumps that might look like pimples or spider bites. These red bumps can turn into deep, painful boils (abscesses) that require surgical draining. If the infection spreads to other parts of the body, such as the bones, joints, bloodstream, heart valves, or lungs, it can cause life-threatening infections.
Most MRSA skin infections can be treated in a doctor's office. Severe infections may require hospitalization and treatment with antibiotics through an IV.