The DRG system, or Diagnostic-Related Groups, is a methodology used by Medicare and some health insurance companies to standardize hospital reimbursement and improve efficiency. The system categorizes hospital visits by severity of illness, risk of mortality, and treatment difficulty, and assigns a predetermined reimbursement amount based on the patient's diagnosis, treatment, and other factors. The DRG system replaces retrospective payments with prospective payments for hospital charges, which can impact the hospital's bottom line and patient outcomes.
| Characteristics | Values |
|---|---|
| Who uses DRG | Medicare and some health insurance companies |
| What is DRG used for | Categorizing hospitalization costs |
| How does DRG affect hospital reimbursement | DRG determines the payment amount hospitals receive for inpatient care |
| How is DRG calculated | Based on the patient's primary and secondary diagnoses, other medical conditions, age, sex, and medical procedures |
| How is DRG payment amount determined | Medicare calculates the average cost of the resources needed to treat people in a particular DRG and adjusts it based on factors like the wage index for a given area |
| Pros of DRG | Standardized reimbursement, improved efficiency, better patient outcomes than fee-for-service payments |
| Cons of DRG | Possible decreased quality of care, upcoding, early discharge, increased odds of hospital readmission |
What You'll Learn
- DRG payment systems are used by Medicare and some health insurance companies
- The DRG system is designed to standardise hospital reimbursement and improve efficiency
- DRGs are based on a patient's diagnosis, treatment, age, sex, and medical procedures
- The DRG system can result in decreased quality of care for patients
- Teaching hospitals and healthcare providers can impact DRGs

DRG payment systems are used by Medicare and some health insurance companies
The DRG system, or "Diagnostic Related Groups", is a means of categorizing and grouping patients with similar clinical diagnoses, treatments, age, sex, and medical procedures. This system is used by Medicare and some health insurance companies to standardize and determine reimbursement rates for hospitalization costs. The DRG system was designed to replace retrospective payments with prospective payments for hospital charges, meaning that a predetermined amount is set based on the patient's DRG. This means that the hospital is paid a fixed amount for the patient's stay, regardless of how many services are received. The DRG system has been applied to inpatient care and, more recently, outpatient surgeries.
When a patient is admitted to the hospital, their stay is classified into one of several hundred DRGs based on their diagnosis, complications, and comorbidities. The length of inpatient stay can also affect the DRG, as longer stays are often associated with more complex medical conditions and more services provided. The patient's discharge status can also impact their DRG, as those discharged to a skilled nursing facility or another type of post-acute care may have a different DRG than those discharged home.
Each DRG is assigned a relative weight based on the average amount of resources required to care for a patient within that group. This base rate is then adjusted based on factors such as the wage index for a given area. For example, a hospital in a high-cost area like New York City will have a higher wage index reflected in the payment rate compared to a rural area.
The DRG system aims to improve efficiency and patient outcomes by standardizing reimbursement rates and bundling payments for inpatient and outpatient services. However, one drawback is the potential for decreased quality of care. The necessity of tests, for example, is determined by an administrative formula that may not fit every patient's unique needs, potentially leading to upcoding or early discharge to save costs.
Psychiatric Hospital Ratings in Ohio: What You Need to Know
You may want to see also

The DRG system is designed to standardise hospital reimbursement and improve efficiency
The DRG system, standing for Diagnostic Related Groups, is a means of standardising hospital reimbursement and enhancing efficiency. The system is designed to group patients with similar clinical diagnoses, treatments, age, sex, and medical procedures. This grouping allows for the standardisation of reimbursement rates, as hospitals are paid a fixed amount based on the DRG category, rather than individual services rendered. The DRG system replaces retrospective payments with prospective payments, simplifying the reimbursement process and providing clarity to patients, healthcare providers, and insurance companies alike.
The DRG system was first introduced in the 1960s as a patient classification scheme. Each DRG category is assigned a relative weight, reflecting the average resources required to treat patients within that group. This relative weighting is a key factor in determining the reimbursement rate for hospitals. The system incentivises hospitals to provide efficient care, as they are reimbursed based on the DRG category, regardless of their actual costs. This can lead to both positive and negative outcomes for patients.
On the one hand, the DRG system may result in decreased quality of care. Administrative formulas may not adequately capture the nuances of individual patient needs, potentially leading to unnecessary tests or early discharge to reduce hospital costs. Additionally, upcoding, or receiving a more severe diagnosis than necessary, can cause undue stress for patients and their families. Furthermore, patients may be discharged too early or transferred to a rehabilitation facility prematurely to save costs, increasing the likelihood of hospital readmission.
However, the DRG system also offers benefits. It encourages hospitals to provide efficient care, utilising resources effectively to treat patients within the DRG framework. This can lead to improved patient outcomes, as hospitals focus on optimising care within the standardised reimbursement structure. Additionally, the DRG system simplifies the understanding of hospitalisation costs for all involved parties, increasing transparency and allowing for more informed decisions regarding treatment options and insurance coverage.
The DRG system has evolved to include outpatient surgeries, reflecting the changing landscape of healthcare delivery. The system continues to be a cornerstone of hospital reimbursement, impacting the financial dynamics of healthcare providers and influencing patient care pathways. While the DRG system aims to strike a balance between standardisation and patient-centric care, ongoing refinement is necessary to ensure that efficiency does not compromise the quality and effectiveness of treatment.
Transplant Preparation: Hospitals Guide and Support Patients
You may want to see also

DRGs are based on a patient's diagnosis, treatment, age, sex, and medical procedures
Diagnosis-Related Groups (DRGs) are used by Medicare and some private insurance companies to determine how much they pay for hospitalizations. The DRG payment system is based on a patient's diagnosis, treatment, age, sex, and medical procedures. When a patient is admitted to a hospital as an inpatient, the hospital assigns a DRG when they are discharged, based on their diagnosis, treatment, and other factors. The DRG system aims to streamline reimbursement for inpatient care by grouping patients with similar clinical characteristics and resource utilization.
The DRG assigned to a patient considers not only the primary diagnosis but also up to 24 secondary diagnoses. This comprehensive approach ensures that the DRG captures the complexity of the patient's condition and the resources required for their treatment. The DRG system also takes into account the patient's treatment needs, including any medical procedures performed during their hospital stay. By considering both the diagnosis and treatment, the DRG system aims to reimburse hospitals based on the overall patient care provided.
Additionally, patient characteristics such as age and sex play a role in determining the DRG. These factors can influence the patient's response to treatment, the likelihood of certain diagnoses, and the resources required for their care. For example, older patients may have different treatment needs or require additional support during their hospital stay, impacting the overall cost of care. Similarly, there may be sex-specific considerations in diagnosis and treatment, as certain conditions or procedures may be more prevalent or vary in their approach between sexes.
The DRG system also considers the specific medical procedures a patient undergoes during their hospitalization. These procedures can vary widely in complexity and cost, impacting the overall reimbursement rate. By including medical procedures in the DRG calculation, the system aims to accurately reflect the resources utilized and compensate hospitals accordingly. However, it's important to note that the DRG system has been primarily designed for inpatient care, and its application to outpatient surgeries is a more recent development.
The DRG payment system has implications for both patients and hospitals. For patients, the DRG system may influence the length of their hospital stay, as hospitals may focus on efficient utilization of resources. On the other hand, hospitals face financial incentives and disincentives based on the DRG reimbursement rates. If a hospital treats a patient more cost-effectively than the DRG rate, it makes a profit on that hospitalization. Conversely, if the hospital spends more than the DRG rate, it incurs a loss. This dynamic encourages hospitals to optimize their treatment approaches and resource utilization.
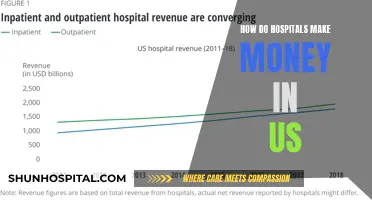
Hospitals' Revenue Streams: Uncovering the US Healthcare System
You may want to see also

The DRG system can result in decreased quality of care for patients
The DRG (Diagnostic-Related Groups) system is intended to standardize hospital reimbursement and ensure that patients receive the care they need while avoiding unnecessary charges. However, it has been argued that the DRG system can result in decreased quality of care for patients. Here are some ways in which the DRG system may lead to reduced quality of care:
- Necessity of tests: The DRG system uses an administrative formula to determine the necessity of tests, which may not fit every patient's unique needs. This could potentially result in patients receiving inadequate or inappropriate care.
- Upcoding: The DRG system may incentivize hospitals to upcode, or provide a more severe diagnosis than necessary, which can cause undue worry and stress for patients and their families.
- Early discharge: Hospitals may discharge patients earlier than medically advisable to save money, potentially compromising patient recovery and leading to increased odds of hospital readmission.
- Channeling resources: To maximize profits, private hospitals may channel their resources towards higher-profit services, potentially compromising care in other areas.
- Focus on low-risk patients: The DRG system may encourage providers to pursue lower-risk patients who require services linked to over-compensation, potentially denying care to high-risk patients or those with complex needs.
- Re-admission rates: The introduction of the DRG system has been associated with increased re-admission rates, which may indicate a decrease in the quality of care provided during the initial hospitalization.
- Quality versus cost: While the DRG system aims to reduce unnecessary costs, it may inadvertently prioritize cost-efficiency over the quality of care delivered.
While the DRG system offers a transparent and cost-effective approach to hospital reimbursement, it is essential to consider its potential impact on patient care. Balancing financial considerations with the delivery of high-quality, patient-centered care remains a complex challenge in healthcare.
Hospitals and Sepsis: What's the Risk?
You may want to see also

Teaching hospitals and healthcare providers can impact DRGs
Teaching hospitals and healthcare providers can impact Diagnostic-Related Groups (DRGs) in several ways. Firstly, they are responsible for assigning the appropriate DRG to patients upon discharge based on their diagnoses and the treatment provided during hospitalization. This assignment is crucial as it determines the reimbursement rate for the hospital. Hospitals receive a fixed payment for each DRG, regardless of their actual spending on treating the patient. Therefore, healthcare providers' ability to efficiently treat patients within the DRG reimbursement rate directly impacts the hospital's financial performance.
Secondly, teaching hospitals and healthcare providers can influence the relative weight assigned to each DRG. Each DRG is given a weight based on the average resources required to care for patients within that group. The expertise and efficiency of healthcare providers can impact the cost and resource utilization associated with treating patients, thereby influencing the relative weight of DRGs.
Additionally, teaching hospitals often have higher labor costs due to their highly educated and specialized workforce. As labor is a significant component of hospital spending, these higher labor costs can impact the overall reimbursement rates for DRGs. Hospitals in different regions may also have varying wage indices, which are considered when determining the DRG payment amounts.
Furthermore, teaching hospitals and healthcare providers can influence the quality of patient care, which may impact readmission rates. For example, early discharge or inadequate treatment may lead to increased odds of hospital readmission. Since 2012, Medicare has implemented a system to penalize excessive readmission rates, affecting the reimbursement methodology and, consequently, the financial implications for hospitals.
Lastly, teaching hospitals and healthcare providers can advocate for changes and adjustments to the DRG system. For instance, during the COVID-19 pandemic, additional codes and a 20% MS-DRG add-on payment were introduced to account for the unique circumstances of treating COVID-19 patients. By actively engaging with healthcare policy and reimbursement systems, teaching hospitals and healthcare providers can impact DRGs and ensure that they reflect the evolving nature of healthcare delivery.
Medication Errors: A Common Hospital Concern?
You may want to see also
Frequently asked questions
DRG stands for Diagnostic Related Groups. It is a system used by Medicare and some health insurance companies to categorize hospitalization costs.
DRGs are based on a patient's primary and secondary diagnoses, other medical conditions, age, sex, and medical procedures. The system categorizes hospital visits by severity of illness, risk of mortality, and treatment difficulty. A predetermined amount is set based on the patient's DRG.
When a patient is discharged from the hospital, Medicare will assign a DRG based on the main diagnosis that caused the hospitalization, plus up to 24 secondary diagnoses. The DRG can also be affected by the patient's treatment and length of stay.
The DRG system was designed to standardize hospital reimbursement and improve efficiency. It replaces retrospective payments with prospective payments for hospital charges. It also helps determine the payment a hospital will receive for providing care to a patient.