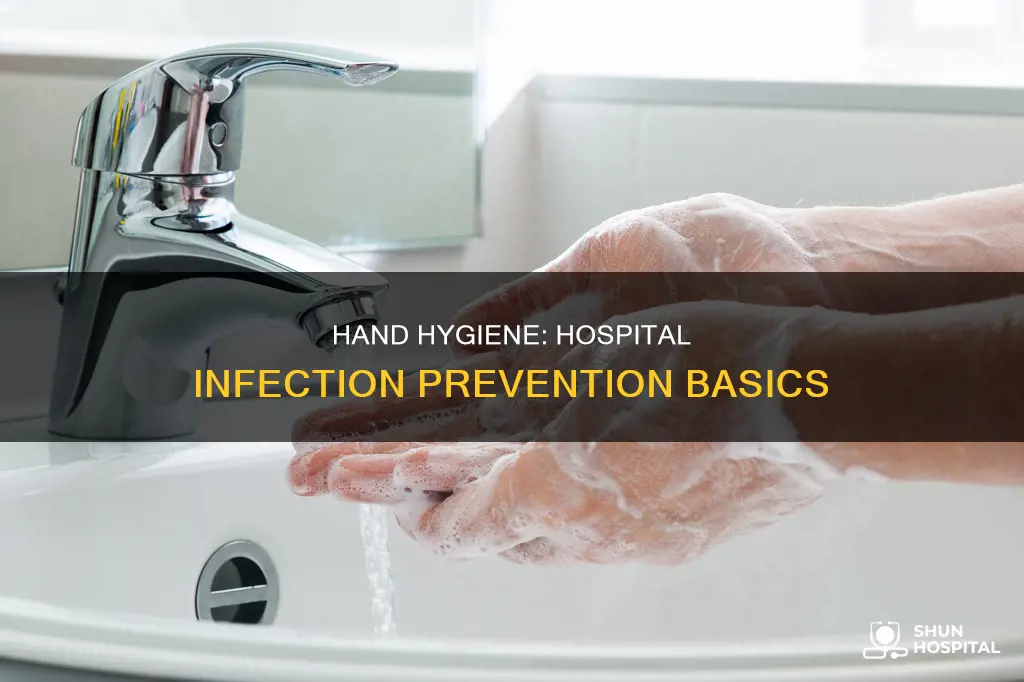
Hand hygiene is an essential practice in healthcare settings, and proper handwashing is critical to preventing infections in hospitals. Healthcare workers come into contact with various surfaces, equipment, and patients, providing opportunities for the spread of germs and infections. By washing their hands, healthcare professionals can reduce the proliferation of microorganisms and the risk of transmitting infections to patients, especially during surgical procedures. This simple yet effective practice helps ensure safe and quality patient care, reducing morbidity and mortality associated with hospital-acquired infections.
| Characteristics | Values |
|---|---|
| Importance | Hand hygiene is the single most important practice in the reduction of the transmission of infection in healthcare settings |
| Effectiveness | Hand washing can prevent the spread of respiratory and diarrhoeal infections, including COVID-19 |
| Germs | Hands can have bad germs that make you sick, but hand washing can prevent the spread of these germs |
| Timing | Wash your hands for at least 15-20 seconds, making sure to clean all areas of your hands |
| Technique | Wet your hands with clean, running water (warm or cold), turn off the tap, apply soap, lather your hands, and scrub |
| Alternatives | If soap and water are not available, use an alcohol-based hand sanitiser with at least 60% alcohol |
| Surgical procedures | Hand hygiene for surgery requires a different set of skills and must remove transient flora and reduce the presence of resident flora |
| High-risk patients | Healthcare professionals must take extra care when caring for immunocompromised patients, as they are at high risk for opportunistic infections |
| Compliance | Compliance with handwashing is high among healthcare workers, but not among the general public |
What You'll Learn
- Alcohol-based hand sanitizers are more effective than soap and water
- Handwashing is essential before and after surgery
- Hand hygiene compliance is poor in many healthcare facilities
- Handwashing with soap removes transient gram-negative bacilli
- Hand hygiene is the most effective way to prevent the spread of infections

Alcohol-based hand sanitizers are more effective than soap and water
Alcohol-based hand sanitizers are highly effective in reducing bacterial load on hands, especially in healthcare settings. They are generally more effective than soap and water in rapidly reducing bacterial load, especially when hands are not visibly dirty. Alcohol-based hand sanitizers are also easier to use during the course of care, for instance, when moving from soiled to clean activities with the same patient or when moving between patients in shared rooms.
Alcohol-based hand sanitizers with 60-95% alcohol concentration are more effective at killing germs than those with lower alcohol concentrations or non-alcohol-based hand sanitizers. They are also safe when used as directed. According to the CDC, alcohol-based hand sanitizers are the preferred way to clean hands in healthcare facilities. They are more effective at killing potentially deadly germs on hands than soap.
Studies have shown that alcohol-based hand sanitizers with higher alcohol content and additional active ingredients are more effective in killing bacteria. They are also more effective in inactivating test viruses, although some soaps showed superior activity against specific viruses. Hand sanitizers are also more effective when hands are generally clean and not heavily soiled or greasy.
However, it is essential to note that the combination of soap and alcohol-based sanitizers offers the most comprehensive approach to hand hygiene. Soap and water are more effective than hand sanitizers at removing certain types of germs, such as Norovirus, Cryptosporidium, and Clostridioides difficile, as well as chemicals. Therefore, it is crucial to consider the specific context and the type of microorganisms when choosing between hand hygiene methods.
Child Hospitalization: Impacting Families, Changing Dynamics
You may want to see also

Handwashing is essential before and after surgery
Handwashing is a simple yet vital practice to prevent the spread of infections and diseases in hospitals. It is especially critical before and after surgery, as surgical sites are highly susceptible to infection.
Before surgery, healthcare workers must ensure proper hand hygiene to protect the patient from potential pathogens. The hands of healthcare providers are a primary source of pathogenic spread, and the inadvertent transfer of microorganisms to a surgical site can result in a surgical site infection, one of the most common hospital-associated infections. Therefore, diligent handwashing before surgery is crucial to reducing the risk of post-operative complications.
The correct hand hygiene steps before surgery involve using either an antimicrobial soap or an alcohol-based hand sanitizer. Alcohol-based sanitizers are more effective at killing potentially harmful germs and are less irritating to the skin. However, when hands are visibly dirty, soap and water are recommended. Proper handwashing technique includes wetting hands with clean, running water, applying soap, and lathering thoroughly, including the backs of the hands, between the fingers, and under the nails, for at least 15 to 20 seconds.
After surgery, handwashing is equally important to prevent the spread of any pathogens that may have been encountered during the procedure. This protects both the healthcare workers and subsequent patients they may come into contact with. Additionally, proper hand hygiene after surgery helps to reduce the risk of healthcare-associated infections, which can have significant health and economic impacts.
Overall, handwashing before and after surgery is a fundamental practice in infection control and patient safety. It is a simple yet powerful tool in preventing the spread of infections and ensuring quality healthcare.
Complaints at Pinderfields Hospital: What You Need to Know
You may want to see also

Hand hygiene compliance is poor in many healthcare facilities
Hand hygiene is essential to providing safe, cost-efficient, and quality care to patients. It is the most effective action to stop the spread of infection and prevent up to 50% of avoidable infections acquired during healthcare delivery. Despite this, hand hygiene compliance is poor in many healthcare facilities.
A study on hand hygiene compliance and associated factors among healthcare providers in Central Gondar Zone public primary hospitals in Northwest Ethiopia found that overall good hand hygiene compliance was only 14.9%. This finding was in line with another study conducted at the University of Gondar Teaching Hospital, Ethiopia (16.5%) and lower than studies conducted in Mali (21.8%), Kuwait (33.4%), India (43.4%), and Black Lion Hospital, Ethiopia (79%). The variation in compliance rates may be due to factors such as the setting of the hospital, sample size, lack of awareness of healthcare-associated infections among healthcare providers, passive Infection Prevention and Control Committees (IPCCs), and the inaccessibility of hand hygiene resources.
Another factor contributing to poor hand hygiene compliance is the difference in hospitals' settings, availability, and accessibility of resources, user acceptance, and cost. For example, in developing countries, the priority given to preventing and controlling healthcare-associated infections is minimal due to a lack of infrastructure, trained manpower, surveillance systems, poor sanitation, overcrowding, and understaffing of hospitals.
Furthermore, behavioral psychology plays a significant role in motivating hand hygiene behaviors. Even during the COVID-19 pandemic, hand hygiene rates initially improved but then decreased back to baseline levels. Emphasizing the importance of proper hand hygiene and its role in preventing infections is crucial to improving compliance rates.
To improve hand hygiene compliance in healthcare facilities, it is essential to implement strategies such as educational programs for patients and healthcare providers, improving ergonomics and staffing ratios, and providing accessible hand hygiene resources. Additionally, continued investment and awareness from system leadership and senior healthcare providers are necessary to set a good example for their subordinates.
US Hospitals: Occupancy Rates and Trends
You may want to see also

Handwashing with soap removes transient gram-negative bacilli
Hand hygiene is an essential practice in hospitals to prevent the spread of infections. While handwashing practices in patient care settings date back to the early 19th century, the importance of hand hygiene has evolved with evidential proof of its effectiveness in reducing pathogens responsible for hospital-acquired infections.
Healthcare providers' contaminated hands are a primary source of pathogenic spread, and proper hand hygiene is crucial to decreasing the proliferation of microorganisms, reducing infection risk, and lowering healthcare costs and lengths of patient stays. According to the Centers for Disease Control and Prevention (CDC), hand hygiene is the most critical practice for reducing infection transmission in healthcare settings.
Handwashing with soap and water is highly effective at removing transient gram-negative bacilli. In hospitals, transient gram-negative bacilli can be effectively eliminated from the hands with a simple soap wash. This is particularly crucial in preventing the spread of infections in healthcare settings. Soap and water can remove nearly all transient gram-negative bacilli in as little as 10 seconds. This simple yet powerful practice plays a vital role in infection control within hospitals.
While soap and water are generally recommended, in certain situations, chlorhexidine may be more suitable for removing specific bacteria. For instance, chlorhexidine is more effective than soap and water in removing transient gram-positive bacteria. Additionally, when dealing with specific pathogens such as Clostridium difficile, Norovirus, or Bacillus anthracis, handwashing is a necessary precaution.
Overall, handwashing with soap and water is a fundamental infection control measure in hospitals, especially effective at removing transient gram-negative bacilli. This simple act significantly contributes to maintaining a safe environment for patients and healthcare workers alike.
Measuring Blood Pressure: Hospital Techniques and Tools
You may want to see also

Hand hygiene is the most effective way to prevent the spread of infections
Hand hygiene is the single most effective way to prevent the spread of infections. The importance of hand hygiene in healthcare settings cannot be overstated, as it is a simple yet powerful tool in the fight against infections. By practising proper hand hygiene, individuals can significantly reduce the transmission of harmful pathogens and keep themselves and those around them safe.
Hand hygiene involves washing hands with soap and water or using an alcohol-based hand sanitiser. In healthcare facilities, alcohol-based hand sanitisers are often preferred due to their effectiveness in killing potentially deadly germs and their ease of use. Proper hand hygiene techniques include ensuring that all areas of the hands are cleaned, including the backs of the hands, fingers, and under the nails. It is also essential to wash hands for at least 15 to 20 seconds.
In a hospital setting, hand hygiene is crucial for preventing hospital-acquired infections (HAIs). Healthcare providers' contaminated hands are a primary source of pathogenic spread, and proper hand hygiene can reduce the proliferation of microorganisms, lowering the risk of infection. This is especially critical for immunocompromised patients who are at high risk for opportunistic infections. Additionally, surgical hand antisepsis is vital to preventing surgical site infections, one of the most common forms of hospital-associated infections.
Hand hygiene is also essential for preventing the spread of infections among patients, their loved ones, and healthcare personnel. Patients and visitors should be encouraged to wash their hands frequently, including before eating, after using the restroom, and after touching surfaces in the hospital room. They should also feel empowered to remind healthcare providers to practise proper hand hygiene and ask about it if they have any concerns.
By implementing hand hygiene improvement programmes, hospitals can prevent up to 50% of avoidable infections acquired during healthcare delivery. These programmes include educational initiatives, ergonomic considerations, and staffing ratios, all contributing to better hand hygiene compliance. Overall, hand hygiene is a simple, cost-effective, and powerful tool in preventing the spread of infections in hospitals and improving patient outcomes.
USC Hospital: A Short Distance From Campus
You may want to see also
Frequently asked questions
Hand washing is one of the most effective ways to prevent the spread of diseases and infections. Germs can live on surfaces for hours and are often passed from person to person through touch. In hospitals, healthcare workers come into contact with patients, equipment, and other items in patient rooms, so hand washing is critical to prevent the spread of illness.
Hand washing prevents the spread of germs, including those that are resistant to antibiotics. Alcohol-based hand sanitizers are more effective at killing potentially deadly germs than soap and water. Washing your hands with soap and water will remove nearly all transient gram-negative bacilli in 10 seconds.
Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap. Lather your hands by rubbing them together with the soap, including the backs of your hands, between your fingers, and under your nails. Scrub your hands for at least 20 seconds.
Wash your hands before preparing or eating food, before touching your eyes, nose, or mouth, after using the restroom, after blowing your nose, coughing, or sneezing, and after touching surfaces in the hospital room.