Hospitals and healthcare providers are required by law to maintain the privacy and security of patient medical records, which contain a variety of personal and health-related information. These records are shared electronically between providers, specialists, pharmacies, and laboratories, and are also used for administrative and financial purposes. While laws vary by state, medical records are typically kept for five to ten years after a patient's last treatment, discharge, or death. Electronic health records (EHRs) are increasingly being adopted due to their convenience, security, and ability to provide a comprehensive view of a patient's health. Patients can also maintain their own personal health records (PHRs), which are controlled by the individual and can be offered through healthcare plans or employers.
| Characteristics | Values |
|---|---|
| Record Retention Period | Most hospitals retain records for 5-10 years, but this varies by state and patient type (adult or minor). Certain Medicaid/Medicare reimbursement regulations require medical records to be available for review for up to 7 years. |
| Record Format | Hospitals use electronic health records (EHRs) or electronic medical records (EMRs) to store patient information digitally. EMRs are digital versions of paper charts, while EHRs provide a broader overview of patient health. |
| Record Security | Hospitals must adhere to strict privacy guidelines, such as HIPAA in the US, to protect patient information. This includes implementing cybersecurity measures to prevent data breaches and identity theft. |
| Record Accessibility | Patients have a right to access their health records and may authorize family or third parties to do so as well. Hospitals may charge a fee for providing record copies, and requests may take up to 45 days to process. |
| Record Transfer | When physicians relocate, they may take medical records with them or leave them with a designated custodian. In group practice changes, physicians should maintain original records and only transfer copies. |
What You'll Learn

Electronic Health Records (EHRs)
An Electronic Health Record (EHR) is a digital version of a patient's medical history. It is maintained by the provider and can be updated in real-time, making it more convenient and efficient than traditional paper records. EHRs may include administrative and clinical data such as demographics, progress notes, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports. They improve upon paper records by making patient information instantly and securely available to authorized users, such as doctors, hospitals, and any loved ones given permission.
EHRs offer several advantages over traditional paper records. They improve healthcare efficiency, save money, and reduce the risk of lost paperwork. They also enable quick access to information, streamline the clinician's workflow, and support other care-related activities through various interfaces. Additionally, EHRs can help prevent hospitalizations among high-risk patients by using data and analytics. They also eliminate the need to track down previous paper records and ensure that data is up-to-date, accurate, legible, and searchable.
While EHRs offer many benefits, there are some challenges to consider. Sharing electronic health records with patients may cause increased confusion or anxiety if they cannot understand or contextualize the information. Many EHRs do not accommodate different educational levels or language needs. Additionally, accessing EHRs requires proficiency with electronic devices, which may be a barrier for some individuals.
It is important to note that patients have a right to access their health records, and hospitals are required by law to protect the privacy of their medical information. Patients can request copies, view the original, or receive a summary of their records. In some cases, patients may need to fill out specific forms or letters to obtain their records, and there may be associated costs.
Bacterial Identification: Hospital Strategies and Techniques
You may want to see also

Privacy and security
To ensure compliance with HIPAA, hospitals must implement reasonable and appropriate administrative, technical, and physical safeguards. This includes securing medical records with lock and key or passcode, limiting access to keys or passcodes, shredding documents containing PHI before disposal, and implementing proper data storage and backup procedures. Hospitals must also provide patients with information on their rights to privacy, what type of PHI will be shared, and why.
In addition to HIPAA, some states have their own, more restrictive rules on the privacy of PHI, particularly regarding sensitive information such as infectious diseases, mental health, genetic disorders, and substance abuse. Hospitals must also comply with federal rules that may be more stringent than HIPAA in certain areas, such as substance abuse and drug addiction records.
To protect patient information, hospitals employ various security measures, including authorization/access control methods, such as single sign-on databases or user access rights lists. They also use automatic account logoff after inactivity, frequent password changes, and physical access controls like chip-based ID cards or biometric features such as fingerprints and facial recognition. These measures help prevent unauthorized access and ensure that only authorized individuals can view patient information.
Furthermore, hospitals must ensure that their computer systems are secure and not accessible to the public or patients. Screens should not be visible, and healthcare providers should log in and log off each time they use the system. All healthcare workers should have unique passwords that are never shared, and they should be trained in security policies and procedures. These policies should include incident reporting, security issue resolutions, and system failure and recovery plans to maintain the integrity of patient information.
Measuring Blood Pressure: Hospital Techniques and Tools
You may want to see also

Patient access
State laws also give patients the right to access their medical records, with some variations between states. For example, in New York, patients have the right to access their medical records, but there are some restrictions on what can be obtained, and fees may be charged. In Connecticut, patients have the right to access their health records, including copies of bills, lab reports, prescriptions, and other technical information. The records must be provided within 30 days of the request, and providers can charge a small fee per page.
It is important to note that patients do not have the right to access all types of records. For example, psychotherapy notes, which are the personal notes of a mental health care provider, are generally not accessible to patients. Additionally, physicians can deny access to personal notes and observations, confidential information, and information that may cause harm to the patient or others.
To request access to medical records, patients typically need to make a written request to their healthcare provider or facility, specifying the information being sought. Patients may also be able to access their records online through secure patient portals or applications, especially with the increasing adoption of electronic health records (EHR) systems.
Overall, maintaining patient access to medical records is crucial for ensuring transparency, enabling patients to review their treatment history, and facilitating continuity of care when transferring between healthcare providers.
The US Hospital Count: A Comprehensive Overview
You may want to see also

Retention periods
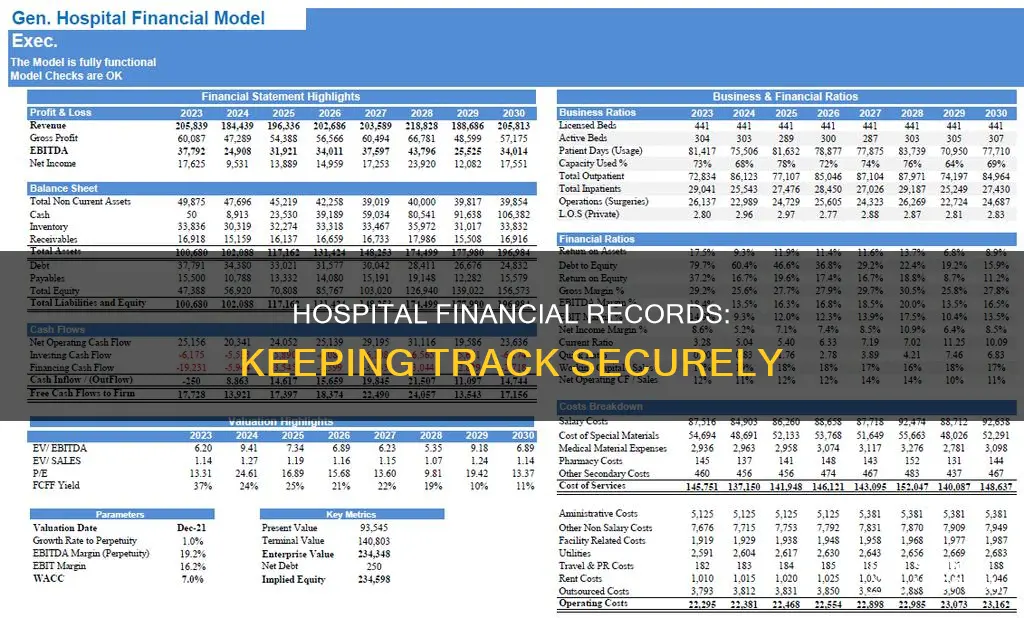
The retention period for hospital financial records varies depending on the state, the type of records, and the patient's age.
HIPAA laws require healthcare providers to retain medical records for six years, while federal law mandates a minimum retention period of seven years after providing the medical service. However, the retention period can vary by state, ranging from five years in Florida to ten years in Illinois and New Jersey. For minors, medical records must be stored until they reach adulthood, with specific variations by state. For example, in New York, medical records for minors must be kept for six years or until one year after they become legal adults, while in New Jersey, medical records for minors must be retained until they turn 23.
Medical billing records are essential for insurance claims and providing a patient's complete medical history. While there is no standard retention period for billing records, the IRS recommends retaining tax and financial records, including bank statements, for at least three years for potential audits and income tax examinations. Additionally, Medicare Advantage (MA) organizations agree to maintain financial records for ten years to accommodate periodic auditing and evaluation by the Centers for Medicare and Medicaid Services (CMS).
Electronic Health Records (EHRs) are digital versions of medical records that improve efficiency, security, and accessibility. While there is no universal retention period for EHRs, they are designed to follow patients throughout their lives and can be retained indefinitely.
Concussion Treatment: Hospital Care and Recovery
You may want to see also

Billing information
In terms of record-keeping, hospitals typically retain billing information as part of a patient's medical record. The duration for which these records are kept can vary depending on local laws and regulations, but it is generally recommended that medical records, including billing information, be kept for at least five to ten years after a patient's last treatment, discharge, or death. This timeframe may be longer in certain circumstances, such as when records are required for legal or financial purposes.
To ensure accuracy and compliance, hospitals often utilise electronic health records (EHRs) or electronic medical records (EMRs). These digital systems provide a comprehensive overview of a patient's billing information, including costs associated with procedures, medications, and hospital stays. EHRs and EMRs enable hospitals to efficiently manage and retrieve billing data, facilitating better financial management and compliance with tax regulations.
The security and privacy of billing information are also crucial considerations. Hospitals must adhere to strict privacy guidelines, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, to protect patient information. This includes safeguarding sensitive data like social security numbers, credit card details, and private health information from unauthorised access and potential identity theft.
In summary, billing information is a critical component of hospital financial records, impacting patients, healthcare providers, and insurance reimbursement processes. Accurate record-keeping, secure storage, and compliance with privacy regulations are essential to maintaining the integrity of billing information in the healthcare industry.
Exploring New York's Extensive Hospital Network
You may want to see also
Frequently asked questions
There is no uniform answer to this. The IRS and most states have a three-year statute of limitations for conducting audits and issuing refunds. However, state guidelines vary, and the minimum amount of time records are kept differs depending on whether the records are held by private-practice medical doctors or hospitals. Most hospitals retain records for five to ten years after a patient's last treatment, last discharge, or death.
You can access your hospital financial records by submitting a request to the hospital's medical records office. You may be charged a fee for these records, and the documents can be sent to you or picked up by you or your attorney.
Hospital financial records are kept securely and privately, with strict privacy guidelines in place. They are often kept electronically, with EHR and EMR systems that help providers track a patient's data over time.