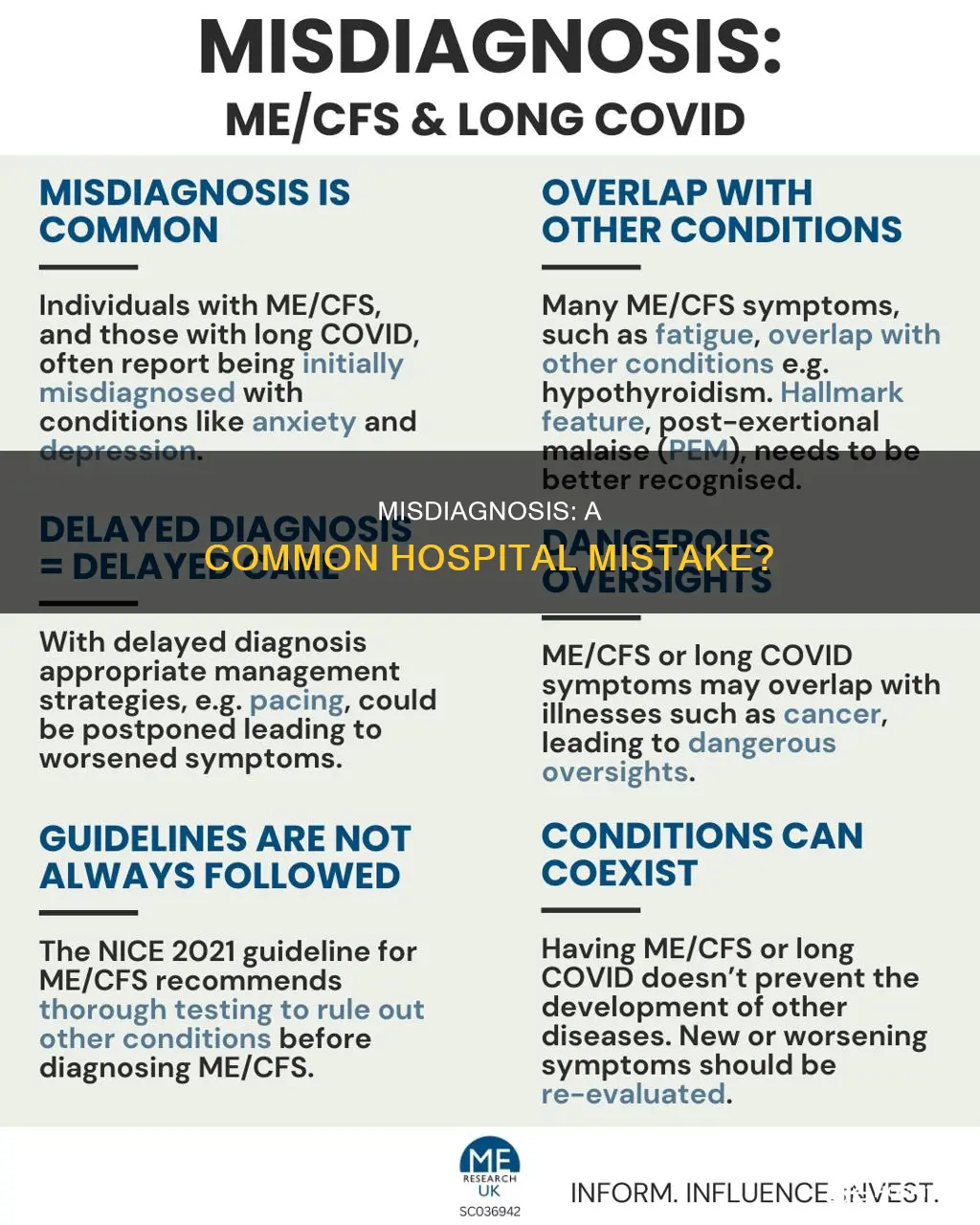
Misdiagnosis is a common issue in hospitals, with diagnostic errors underlying a significant proportion of adverse events in hospital practice. In the United States, approximately 12 million people are affected by medical diagnostic errors each year, with 40,000 to 80,000 deaths attributed to complications from these misdiagnoses. Diagnostic errors can occur due to various factors, including cognitive biases, system failures, and human-cognitive failures, such as faulty data gathering and inadequate reasoning. While not all misdiagnoses result in harm, some cases can have serious or even fatal consequences, emphasizing the critical need for accurate and timely diagnoses in healthcare settings.
| Characteristics | Values |
|---|---|
| Percentage of adverse events in hospital practice caused by diagnostic errors | 10% to 14% |
| Leading cause of medicolegal claims in the USA | Misdiagnosis (26%) |
| Number of people affected by medical diagnostic errors in the USA annually | 12 million |
| Number of people who die from complications from misdiagnoses in the USA annually | 40,000 to 80,000 |
| Probability of misdiagnosis for women and minorities | 20% to 30% higher |
| Percentage of diagnostic adverse events influenced by human cognitive factors in Dutch study | 96% |
| Percentage of diagnostic adverse events influenced by human cognitive factors in American study | 74% |
| Percentage of diagnostic errors caused by system-based failures in Dutch study | 25% |
| Percentage of diagnostic errors caused by system-based failures in American study | 65% |
| Percentage of diagnosis-related claims by volume in CRICO's analysis | 20% |
| Percentage of indemnity payments in CRICO's analysis | 27% |
| Setting with the highest incidence of diagnostic errors in CRICO's analysis | Ambulatory care (56%) |
| Settings with lower incidence of diagnostic errors in CRICO's analysis | Inpatient care (28%) and emergency department (16%) |
| Example of diagnostic errors in inpatient setting | Myocardial infarction, cardiac events, complications of care, and infections/sepsis |
| Example of a condition that is often misdiagnosed | Endometriosis |
| Example of a serious consequence of misdiagnosis | Missed or delayed cancer diagnosis |
What You'll Learn
- Misdiagnosis in the US affects 12 million people annually, with 40,000-80,000 deaths
- Diagnostic errors underlie 10-14% of adverse events in hospitals
- Misdiagnosis claims represent 20% of cases by volume and 27% of indemnity payments
- Women and minorities are 20-30% more likely to be misdiagnosed
- Cognitive biases and human-cognitive failures are factors in misdiagnosis

Misdiagnosis in the US affects 12 million people annually, with 40,000-80,000 deaths
Misdiagnosis in the US healthcare system is a significant issue, affecting millions of people annually and resulting in thousands of deaths. According to a recent report, approximately 12 million people in the United States fall victim to medical diagnostic errors each year, with an estimated 40,000 to 80,000 deaths occurring due to complications arising from these misdiagnoses. This figure represents the number of people who suffer serious harm as a consequence of diagnostic errors, with the actual number of errors likely being much higher.
The impact of misdiagnosis extends beyond the physical consequences, as it can also lead to psychological and emotional distress for patients and their families. The financial implications can also be significant, resulting in additional costs for both the patients and the healthcare system. The emotional toll of dealing with a misdiagnosis can be profound, leading to anxiety, fear, and a breakdown of trust in the medical profession. Furthermore, the financial burden of treating complications arising from misdiagnosis can be substantial, often requiring additional tests, medications, and procedures that could have been avoided with an accurate initial diagnosis.
Several factors contribute to the high rate of misdiagnosis in the US. One of the primary reasons is the complexity of the healthcare system, which can lead to fragmented care and a lack of coordination between different healthcare providers. Additionally, the high cost of healthcare in the US may deter people from seeking medical help until their condition becomes more severe, making accurate diagnosis more challenging.
Diagnostic errors can occur due to a variety of reasons, including human cognitive factors and system failures. Human cognitive factors, such as faulty data gathering, inadequate reasoning, and faulty verification, play a significant role in misdiagnosis. System failures, including technical and organizational malfunctions, can also contribute to diagnostic errors. Additionally, individual physicians may be reluctant to acknowledge their mistakes, further compounding the issue. Furthermore, diagnostic errors may go undetected or unreported, hindering efforts to address this critical issue effectively.
To reduce the incidence of misdiagnosis, it is essential to implement systemic changes and improve diagnostic processes. This includes investing in new technologies, such as AI-powered systems, that can assist doctors in making more accurate diagnoses. Additionally, there is a need for better documentation and standardization of medical records, ensuring that all relevant information is readily available to healthcare providers. By addressing these issues, the US healthcare system can improve patient safety, reduce adverse outcomes, and enhance the overall quality of care.
Accreditation Systems: Improving Hospital Performance and Patient Care
You may want to see also

Diagnostic errors underlie 10-14% of adverse events in hospitals
Diagnostic errors are a significant contributor to adverse events in hospitals, accounting for an estimated 10-14% of all adverse events. This highlights the critical need to improve diagnostic processes and patient safety measures.
Various factors can lead to diagnostic errors, and these can be categorised into three main groups: no fault, system-based, and human-cognitive. 'No fault' situations include unusual disease presentations or patients providing unclear symptom descriptions. System errors encompass technical and organisational failures, while human-cognitive failures involve faulty data gathering, inadequate reasoning, and faulty verification. Cognitive biases, in particular, can significantly influence diagnostic conclusions.
The incidence of diagnostic errors varies across medical specialties. For instance, diagnosis-related claims in obstetrics constituted 9% of total claims, while in paediatrics, they accounted for 61%. Furthermore, diagnostic errors are more prevalent in ambulatory care settings (56%) compared to inpatient (28%) or emergency department settings (16%).
The impact of diagnostic errors is profound, with an estimated 12 million people in the United States affected by medical diagnostic errors annually. Misdiagnosis is a leading cause of medicolegal claims, and it is estimated that 40,000 to 80,000 people die each year from complications arising from these errors.
Despite the high occurrence and severe consequences of diagnostic errors, there has been limited research into improving diagnostic mechanisms. This area of patient safety requires urgent attention, with misdiagnosis being described as 'the next frontier for patient safety'.
University Hospital: Tamarac's Busy Medical Hub
You may want to see also

Misdiagnosis claims represent 20% of cases by volume and 27% of indemnity payments
Misdiagnosis is a significant issue within the healthcare industry, with diagnostic errors underlying about 10% of adverse events occurring in hospitals. In the United States, 12 million people are affected by medical diagnostic errors annually, resulting in an estimated 40,000 to 80,000 deaths. Misdiagnosis claims represent a substantial proportion of medical negligence cases, with 20% of cases by volume and 27% of indemnity payments attributed to diagnostic errors. This highlights the financial and legal implications of misdiagnosis, which can result in costly compensation claims for healthcare providers.
The impact of misdiagnosis extends beyond financial consequences. Patients affected by misdiagnosis may endure painful and potentially fatal outcomes due to receiving improper or delayed treatment. It is important to note that not all misdiagnosis cases result from negligence, as some may be categorised as "no fault," involving unusual disease presentations or confusing patient symptom descriptions. However, when negligence is involved, it typically constitutes a breach of the duty of care, where healthcare providers fail to meet accepted standards, such as ordering appropriate tests or interpreting symptoms correctly.
To establish a misdiagnosis claim, three core elements must be present: negligence, breach of duty, and harm to the patient. The value of misdiagnosis claims can vary significantly, influenced by factors such as the severity of harm, medical expenses, and loss of income or earning capacity. While some cases result in modest settlements, others have led to multimillion-dollar awards, emphasising the financial implications for healthcare providers and insurers.
To address the issue of misdiagnosis, improvements in diagnostic processes are essential. This includes encouraging analytical reasoning among healthcare professionals, enhancing data gathering and verification practices, and promoting reflection on past errors to prevent future mistakes. By implementing these measures, healthcare providers can strive to reduce misdiagnosis rates, improve patient outcomes, and mitigate the financial and legal consequences associated with diagnostic errors.
In summary, misdiagnosis claims representing 20% of cases by volume and 27% of indemnity payments underscore the significance of diagnostic errors in the healthcare industry. This situation has led to financial, legal, and, most importantly, human impacts, emphasising the critical need for improvements in diagnostic processes to enhance patient safety and reduce adverse outcomes.
Community Hospitals: Legal Setup Explained
You may want to see also

Women and minorities are 20-30% more likely to be misdiagnosed
Misdiagnosis is a significant issue in healthcare, with an estimated 795,000 patients a year dying or becoming permanently disabled due to diagnostic errors in the United States. Within this context, it is particularly concerning that women and racial and ethnic minorities are 20-30% more likely to be misdiagnosed than white men. This disparity has been highlighted in various studies and has been attributed to several factors.
One factor contributing to the higher misdiagnosis rate among women and minorities is implicit bias in healthcare professionals. Despite most doctors not deliberately discriminating, many exhibit unconscious biases that influence their diagnostic decisions. For example, Black people with depression are more likely to be misdiagnosed with schizophrenia, and minorities are often less likely to receive early dementia diagnoses, limiting their treatment options. The impact of these biases can be seen in the story of Charity Watkins, a Black woman who experienced exhaustion and breathlessness after giving birth. Her concerns were dismissed as postpartum depression and the flu, and when she thought she was having a heart attack, she waited 5.5 hours in a North Carolina hospital without seeing a doctor.
Another factor is the disparity in healthcare access. Minority patients are often less likely to be insured and face challenges in accessing high-quality hospitals, potentially contributing to delays in diagnosis and treatment. This issue was highlighted by Monika Goyal, an emergency physician who found that Black children with appendicitis were less likely to receive an accurate diagnosis than their white peers, even when visiting the same hospital.
The consequences of misdiagnosis can be severe, and researchers have deemed it an urgent public health problem. For instance, the misdiagnosis of heart attacks can lead to permanent disability or death, with Black women facing a higher risk of heart failure due to the weakening of the heart muscle. Additionally, misdiagnosis contributes to medico-legal claims, with diagnostic errors now rivaling surgical accidents as the leading cause of such claims in the United States.
To address this issue, experts emphasize the importance of getting to know the patient's story, asking follow-up questions, conducting examinations, and ordering basic tests. By improving diagnostic processes and addressing implicit biases, the healthcare system can strive to reduce the disproportionate impact of misdiagnosis on women and minorities.
Roseburg VA Hospital: Size and Scope
You may want to see also

Cognitive biases and human-cognitive failures are factors in misdiagnosis
Misdiagnosis is a significant issue in healthcare, with diagnostic errors underlying about 10% of adverse events in hospitals. In the United States alone, 12 million people are affected by medical diagnostic errors annually, resulting in an estimated 40,000 to 80,000 deaths. While the exact rates of misdiagnosis may vary across different healthcare systems and countries, it is evident that cognitive biases and human-cognitive failures play a crucial role in these errors.
Cognitive biases are inherent tendencies that influence our decision-making processes. In medicine, these biases can affect clinical reasoning and lead to diagnostic inaccuracies, mismanagement, and mistreatment. Confirmation bias, anchoring bias, and availability bias are examples of cognitive biases that can contribute to wrong-site surgeries, delays in treatment, and other adverse outcomes. For instance, anchoring bias occurs when an individual relies too heavily on the first piece of information they receive, potentially ignoring subsequent information that could lead to a more accurate diagnosis.
Human-cognitive failures, on the other hand, refer to errors in the cognitive processes involved in gathering data, reasoning, and verification. This includes faulty data gathering, such as inaccurate patient history taking or physical examinations, inadequate reasoning skills, and faulty verification of test results or diagnostic criteria. These failures can be due to factors such as time constraints, lack of analytical thinking, or insufficient training, which can increase the likelihood of misdiagnosis.
Several studies have highlighted the impact of cognitive biases and human-cognitive failures on diagnostic errors. A Dutch study found that human cognitive factors played a significant role in 96% of diagnostic adverse events, while an American study reported cognitive errors in 74% of cases. These biases and failures can have severe consequences, not only for patients but also for healthcare providers. When errors lead to adverse events, healthcare professionals may experience second victim syndrome, characterized by shame, guilt, anxiety, and even depression.
To reduce the impact of cognitive biases and human-cognitive failures on misdiagnosis, several strategies can be employed. Healthcare providers can increase their self-awareness by identifying their implicit biases, personal triggers, and situational triggers in the workplace. By recognizing these factors, providers can actively work to minimize their impact on clinical decision-making. Additionally, conducting incident investigations, utilizing quality assessment tools, and promoting a culture of reflective practice can help identify and address cognitive biases and human-cognitive failures, ultimately improving diagnostic accuracy and patient outcomes.
Hospital Ship Comfort: Massive Floating Medical Facility
You may want to see also
Frequently asked questions
Diagnostic errors underlie a significant proportion of adverse events in hospital practice. In the United States, 12 million people are affected by medical diagnostic errors each year. An estimated 40,000–80,000 people die annually from complications from these misdiagnoses.
There are several reasons why a doctor may make a diagnostic mistake. These can be categorised into three groups: no fault, system-based, and human-cognitive. 'No fault' includes unusual or silent presentations of a disease and cases in which patients provided confusing descriptions of symptoms. 'System errors' include technical and organisational malfunctions, and human-cognitive failures include the faulty gathering of data, inadequate reasoning, and faulty verification.
A wrong diagnosis can lead to a medical malpractice lawsuit. Not all misdiagnoses result in harm, but serious or even fatal consequences can follow. For example, a missed or delayed cancer diagnosis can give the cancer time to grow and spread, sometimes making effective treatments more difficult or impossible.
If you receive a wrong diagnosis, you can bring a misdiagnosis malpractice claim or lawsuit. To do so, you must prove that a doctor in a similar specialty, under similar circumstances, would not have misdiagnosed your condition.







