Breast cancer screening is a way to check for cancer before any signs or symptoms of the disease are present. The goal of screening is to detect cancer early on, when it is easier to treat. Screening tests for breast cancer include mammograms, clinical breast exams, and breast self-exams. Mammograms are low-dose X-rays of the breast that can detect tumours that are too small to feel. Clinical breast exams are performed by a doctor or nurse who uses their hands to feel for lumps or other changes. Breast self-exams involve examining one's own breasts to get familiar with how they normally look and feel, so that any changes can be noticed. While screening tests can help detect breast cancer early, it's important to note that they do not reduce the risk of dying from the disease.
| Characteristics | Values |
|---|---|
| Purpose | To detect and treat breast cancer early, improving the chances of survival |
| Screening tests | Mammograms, breast MRIs, clinical breast exams, breast self-exams |
| Screening recommendations | Women aged 40+ should get mammograms every 1-2 years; women with a family history of breast cancer should assess their risk with a health care provider |
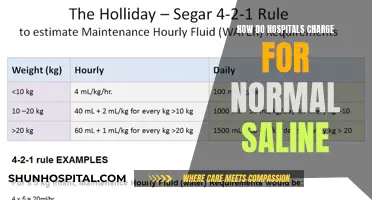
| Mammogram | Low-dose X-rays to take pictures of the breast; can detect tumors too small to feel |
| Breast MRI | Uses magnets and radio waves to take pictures of the breast; used with mammograms for women at high risk |
| Clinical breast exam | Performed by a doctor or nurse to feel for lumps or changes |
| Breast self-exam | Recommended by doctors to be done monthly starting in late teens or early 20s to familiarize oneself with how breasts normally look and feel |
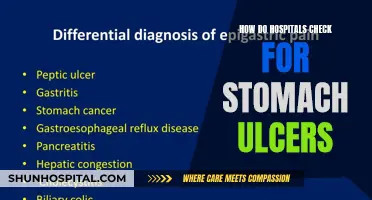
| Biopsy | The only way to know for sure if it's cancer; done when imaging tests or physical exams show a breast change that may be cancer |

Mammograms
However, mammograms are not perfect and do have some drawbacks. They may miss some breast cancers, and if something suspicious is detected, further tests will be needed to confirm whether it is cancerous. Mammograms also expose patients to radiation, although the amount is small, and there may be risks associated with repeated X-rays. Mammograms may also be less effective for women with dense breasts, who are at an increased risk of breast cancer.
In recent years, a newer type of mammogram called digital breast tomosynthesis (3D mammography) has become more common. Studies suggest that 3D mammograms can lower the chance of being called back for follow-up testing and are better at detecting breast cancer, especially in women with dense breasts. However, they are often more expensive than standard 2D mammograms, and the added cost may not be covered by insurance.
Michigan Medicine: A Sprawling Healthcare Hub
You may want to see also

Breast self-examinations
While mammograms are the best screening tool to detect breast abnormalities, breast self-examinations are a great way to be familiar with your own breasts and detect any changes. It is important to note that breast self-examinations are not a diagnostic tool for breast cancer. Only a trained healthcare provider can confirm if a lump you feel during a self-exam is potentially harmful.
By looking at and feeling your breasts regularly, you can better notice changes in your breasts or detect when something feels different. This helps you get an idea of how your breasts normally feel and look, so you can spot any problems. For example, a lump on your breast could be a sign of breast cancer. Finding that lump could allow you to get checked out with a mammogram earlier than you might have otherwise.
- Remove your shirt and bra.
- Use your right hand to examine your left breast, then switch hands and do the same for your right breast.
- With the pads of your three middle fingers, press on every part of one breast using light, medium, then firm pressure. Feel for any lumps, thick spots, or other changes. A circular pattern may help ensure you check every spot.
- Press the tissue nearest your armpit, and be sure to check under your areola (the area around your nipple). Then, squeeze your nipple to check for discharge.
- Repeat the steps on the other side.
- Lie down and put a pillow under your right shoulder. When you lie down, your breast tissue spreads more evenly, making it easier to feel for changes, especially if you have large breasts.
Warning signs of breast cancer
Some warning signs of breast cancer to look out for during a breast self-examination include:
- Inverted nipple or nipples that stop sticking out
- Redness, soreness, a rash, or swelling on your breasts
- Dimpling or puckering (like an orange peel) of the skin of your breasts
- Irregular nipple discharge
Remember, while breast self-examinations are a great way to be aware of any changes in your breasts, they do not reduce the risk of dying from breast cancer. The best way to detect breast cancer early is to get regular screening tests, such as mammograms, which can find breast cancer at an early stage when treatment is most likely to be successful.
Jackson Avery: The Downfall of Seattle Grace Hospital
You may want to see also

Clinical breast exams
A clinical breast exam (CBE) is a physical examination of the breasts by a healthcare professional. It is usually performed by a doctor or nurse practitioner, but other medical staff can also carry it out, as long as they are well-trained in the technique. The healthcare provider carefully feels the patient's breasts, underarms, and the area below the collarbone for any changes or abnormalities, such as lumps. The patient is examined visually while sitting up and physically while lying down.
During a CBE, the healthcare provider will note the size, shape, and texture of any lumps found. They will also check to see if the lump moves easily. Benign lumps often feel different from cancerous ones, but any lump discovered will likely require further diagnostic measures. For example, lumps that are soft, smooth, round, and movable are likely benign tumors or cysts. On the other hand, a hard and oddly-shaped lump that feels firmly attached within the breast is more likely to be cancerous, but further tests are needed to diagnose the problem.
CBE is a key step in the diagnosis and surveillance of benign and malignant breast diseases. It provides important information that is used in the workup and management of many breast diseases. While CBE can help find breast cancer early, it is not recommended for average-risk women by some organizations, including the American Cancer Society. Instead, regular mammograms are advised for this group, as they can detect cancer earlier and lead to more successful treatment outcomes.
However, for women with abnormal findings on mammograms or those at increased risk for breast cancer, CBE is often recommended as part of their annual screening. It is important to note that CBE does not reduce the risk of dying from breast cancer, and some organizations do not recommend it for screening purposes due to a lack of scientific evidence. Nevertheless, it can be a valuable tool when used in conjunction with other screening methods and for certain high-risk groups.
Nurses' Battle: Hospital-Acquired Infections' Impact
You may want to see also

Breast MRIs
Breast cancer screening involves checking a woman's breasts for cancer before any signs or symptoms of the disease are present. Screening can help find breast cancer early on, when it is easier to treat. While breast self-exams are no longer recommended by all expert groups due to the possibility of over-treatment of benign lumps, breast self-awareness is still important. Being familiar with how your breasts normally look and feel can help you notice any changes, such as lumps or pain, which may be a concern.
Breast Magnetic Resonance Imaging (MRI) is a procedure that uses large magnets and radio waves to create detailed images of the inside of the breast. It is used to screen for breast cancer in women who are at high risk, often in conjunction with a mammogram. MRI can help detect small abnormalities that may be missed by mammography or ultrasound, especially in women with dense breast tissue, implants, or scar tissue. Additionally, it can be used to determine the size and location of cancerous lesions and check for tumours in the other breast.
MRI has some limitations as a screening tool. It may appear abnormal even in the absence of cancer, leading to false positives and unnecessary further testing or biopsies. Additionally, MRI has historically struggled to identify calcifications or tiny calcium deposits that can indicate breast cancer. As such, it is not recommended as a standalone screening test for women at average risk of breast cancer.
The American Cancer Society (ACS) and other expert organisations have developed screening guidelines for women based on their risk level. Women at average risk are those without a personal or strong family history of breast cancer, genetic mutations such as BRCA1 or BRCA2, or prior chest radiation therapy before the age of 30. ACS guidelines recommend that women between 40 and 44 have the option to start screening with a mammogram every year, while women 45 to 54 should have yearly mammograms. Women 55 and older can switch to mammograms every other year or continue yearly screenings.
For women at high risk, screening options may include MRI in addition to mammograms. The ACS and other organisations consider high-risk women to be those with BRCA1 or BRCA2 mutations, a first-degree relative with these mutations, or a 20-25% or greater lifetime risk of breast cancer based on risk assessment tools.
Ephrata Hospital Tragedy: Carl Millinder's Unfortunate End
You may want to see also

Biopsies
A breast biopsy is a common procedure used to determine whether a suspicious area in the breast could be cancerous. It is the only way to confirm a breast cancer diagnosis. However, it's important to note that most biopsy results are not cancerous, and having a biopsy does not necessarily mean you have breast cancer.
There are several types of breast biopsies, but they typically involve either a biopsy needle or surgery. The type of biopsy performed depends on various factors, and a healthcare provider will recommend the most suitable option. Before the biopsy, a patient may undergo imaging tests or image-guided procedures to pinpoint the area of the breast that will be checked for signs of cancer.
- Fine needle aspiration (FNA): This involves using a very thin, hollow needle attached to a syringe to withdraw a small amount of tissue or fluid from the suspicious area.
- Core needle biopsy (CNB): This uses a larger hollow needle to obtain a sample of breast tissue. This type of biopsy is often preferred if breast cancer is suspected.
- Excisional biopsy (lumpectomy): This is a surgical procedure to remove all potentially cancerous tissue, as well as some surrounding normal tissue, to ensure all cancer cells are extracted.
- Incisional biopsy: This surgical procedure involves removing only a part of the abnormal tissue in the targeted area.
In some rare cases, surgery may be required to remove all or part of a lump for further testing. This is known as a surgical or open biopsy. During this procedure, the surgeon may also check the lymph nodes under the arm to determine if the cancer has spread.
Doctors' Impact on Hospital Costs: A Complex Dynamic
You may want to see also
Frequently asked questions
Hospitals use a variety of tests to check for breast cancer, including mammograms, MRIs, ultrasounds, and biopsies.
A mammogram is a low-dose X-ray of the breast that can detect small tumors before they can be felt. Mammograms are generally recommended for women starting at age 40 and can be repeated every 1-2 years.
A breast MRI uses magnets and radio waves to take pictures of the breast. It is used along with mammograms for women at high risk of getting breast cancer.
The frequency of breast exams depends on your age and risk factors. Women aged 20 to 39 should be examined by a health professional every three years, while women aged 40 and over should be examined annually.