Hospitals have protocols in place to deal with mass casualty incidents (MCIs), which are becoming increasingly common due to both manmade and natural disasters. These protocols include calling in more staff, utilising spare equipment, and clearing non-acute patients. Triage plays a crucial role, with patients categorised by the severity of their injuries using a colour-coded system. Hospitals also coordinate with other agencies and responders, such as first responders, paramedics, and specialised rescue teams, to manage the influx of patients and ensure efficient treatment and transport. The success of these protocols depends on factors such as staff training, infrastructure, and coordination with community organisations.
| Characteristics | Values |
|---|---|
| Preparation | Hospitals have mass casualty incident protocols in place, including calling in more staff, using extra equipment, and clearing non-acute patients. |
| Triage and Treatment | Patients are triaged and treated according to priority, with red-tagged patients receiving immediate attention, followed by yellow, green, and black-tagged patients. |
| Transportation | Mutual aid ambulance services, first responder units, and EMS personnel provide transportation and evacuation of MCI patients as per regional policies. |
| Coordination | Multiple agencies and responders, including certified first responders, paramedics, EMTs, and ground ambulances, coordinate to provide patient care and transportation. |
| Resource Allocation | The allocation of resources is based on patient triage, with the most critical patients receiving priority treatment. |
| Staff Training | Hospitals train staff on a basic all-encompassing plan, with operational details tailored to the specific incident and local risk factors. |
| Infrastructure | Hospitals ensure they have the necessary infrastructure, including trauma centers with varying levels of resources and capabilities, to respond effectively to mass casualty incidents. |
| Field Hospitals | Governments maintain complete field hospital setups that can be deployed within their jurisdiction in 12-24 hours, while interim-care centers can be set up more quickly. |
| Security | Security measures are implemented, including scene identification vests and, in the case of terrorist incidents, ballistic tactical vests. |
| Waiting Times | Hospitals aim to minimize waiting times for critical treatment, especially for surgical interventions, as they are closely related to patient outcomes. |
What You'll Learn
- Hospitals have emergency plans for mass casualty incidents (MCIs)
- Triage systems are used to categorise patients by priority
- Hospitals increase staff and resources to deal with MCIs
- Hospitals coordinate with other agencies and responders
- Hospitals prepare for a range of disasters, both natural and manmade

Hospitals have emergency plans for mass casualty incidents (MCIs)
Hospitals with emergency departments have emergency plans in place for mass casualty incidents (MCIs). These plans are designed to manage a large influx of patients and ensure they receive timely and effective treatment. The plans cover various aspects, including staffing, resources, patient triage, treatment, and coordination with other agencies.
One critical component of hospital emergency plans is the activation of additional medical staff. Hospitals may call in more doctors, nurses, and other healthcare professionals to handle the increased patient load during an MCI. This ensures that there are enough hands-on deck to provide care and treatment to all patients.
Another important aspect is resource allocation and management. Hospitals may pull out extra equipment, supplies, and medications from storage to meet the increased demand. This includes ensuring that there are enough beds, medical devices, and pharmaceuticals to treat a high volume of patients.
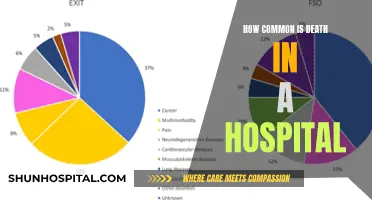
Patient triage is also a crucial element of MCI plans. Hospitals implement triage systems to assess and prioritize patients based on the severity of their injuries. Patients are typically categorized into four groups: minor (green), delayed (yellow), immediate (red), and expectant (black). This triage system helps ensure that those with the most critical and immediate needs receive treatment first.
Furthermore, hospitals coordinate with external agencies and responders during MCIs. This includes collaboration with emergency medical services, first responder units, law enforcement, transportation agencies, and other healthcare facilities. Effective coordination ensures efficient patient transport, scene management, security, and resource allocation.
To enhance their preparedness, hospitals also conduct training and simulations to practice their MCI plans. These exercises help identify areas for improvement and optimize their response capabilities. By training staff on an all-encompassing plan with adaptable operational details, hospitals can better respond to various types of disasters, including natural disasters, epidemics, and traumatic events.
Internal Bleeding: Hospital Detection Techniques and Procedures
You may want to see also

Triage systems are used to categorise patients by priority
Hospitals with emergency departments have mass casualty incident (MCI) protocols in place to deal with a large number of casualties. These protocols involve calling in more staff, preparing extra equipment, and clearing non-acute patients. Triage systems are an essential component of MCI protocols, allowing medical personnel to categorise patients by priority and ensure efficient treatment and resource allocation.
The START adult algorithm is commonly used in MCI triage and consists of four categories: minor (green), delayed (yellow), immediate (red), and expectant (black). Patients tagged as "minor" or "walking wounded" have relatively minor injuries and are unlikely to deteriorate rapidly. They may even be able to assist in their care. Those with delayed or yellow tags require attention but can wait longer than those with red tags. Patients with red tags are the most critical and require immediate treatment. Finally, those with black tags have the lowest priority and are expected to survive with minimal intervention.
Each coloured triage category has its own treatment area, often designated by coloured markers such as tarpaulins, tape, signs, or tents. This colour-coded system helps organise and streamline patient treatment, ensuring that those with the most severe injuries receive immediate attention. The triage system also aids in efficient resource allocation, as medical personnel can quickly identify the priority level of each patient and allocate resources accordingly.
The use of triage tags and colour-coded systems helps to standardise the triage process and improve efficiency during MCI responses. It enables medical personnel to make rapid assessments and ensure that patients receive the appropriate level of care based on their condition. This system is particularly crucial when dealing with a high volume of casualties, as it helps to prioritise treatment and optimise the use of limited resources.
In addition to the START triage system, other aspects of MCI response include scene control, security, and coordination with various agencies. Scene identification vests are distributed to key personnel, and safe areas are established for staging, triage, and treatment, separate from the accident scene or "hot zone." Law enforcement and safety officers play crucial roles in maintaining security and assessing hazards to ensure the safety of both victims and responders. Effective coordination between multiple agencies, such as emergency medical services, transportation, and specialised rescue teams, is also essential in managing MCI effectively.
The Complex System of Hospital Operations
You may want to see also

Hospitals increase staff and resources to deal with MCIs
Hospitals with emergency departments will have a mass casualty incident (MCI) protocol which they initiate to deal with MCIs. This involves calling in more staff, using extra equipment, and clearing non-acute patients from the hospital. Hospitals may also send doctors to the scene of the incident to assist with triage, treatment, and transport of injured persons.
The increasing frequency and intensity of MCIs have compelled hospitals to enhance their disaster preparedness plans. These plans cover immediate patient care, staff roles, security, and coordination with community organizations. Hospitals train their staff on a basic all-encompassing plan, with operational details tailored to the specific incident and local risk factors. This allows for flexibility and adaptability, ensuring that job titles and status do not hinder the effective utilization of each individual's capabilities during an MCI.
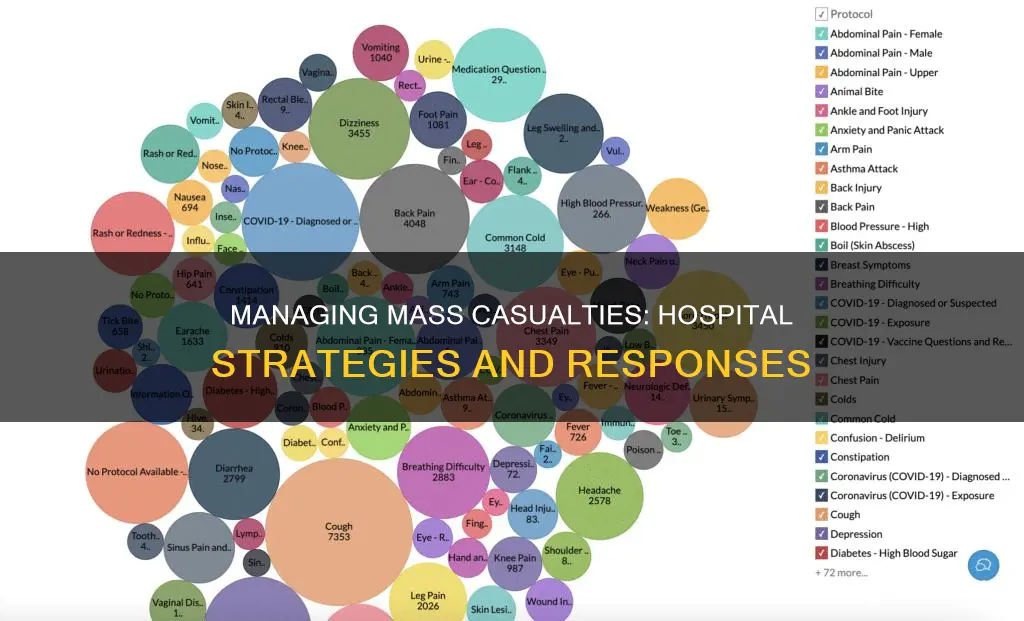
To manage the influx of patients during an MCI, hospitals use triage systems to prioritize treatment. Patients are categorized based on the severity of their injuries, with red tags indicating immediate attention, followed by yellow, green, and black tags. Treatment areas are designated using colored markers, and patients are reassessed upon arrival for stabilization before being transported to the appropriate facility or released.
In addition to increasing staff and utilizing triage systems, hospitals also face challenges in allocating resources effectively. This includes optimizing the staff mix, such as the number of radiologists and rotation physicians, to minimize waiting times for critical treatments. Hospitals coordinate with regional medical systems to manage patient transfers and accommodate surges in emergent and non-emergent cases. These coordinated efforts are crucial in ensuring that patients receive timely and appropriate care during MCIs.
Senior Living: Proximity to Hospitals for Peace of Mind
You may want to see also

Hospitals coordinate with other agencies and responders
Hospitals with emergency departments will have a mass casualty incident (MCI) protocol that they initiate as soon as they receive notification of an MCI in their community. This includes coordinating with other agencies and responders.
The first available responder squad on the scene is responsible for assessing the extent of the catastrophe, providing a scene report, and alerting nearby hospitals to determine resource and bed availability. The Massachusetts Department of Public Health recommends using the "METHANE" mnemonic to quickly and efficiently gauge the extent of the MCI. This includes assessing the type of incident, access for emergency services, and the number of casualties.
Certified first responders or emergency medical responders may arrive as part of local emergency medical services or on their own. They assist with patient care, including triage and treatment at the scene, and transport to hospitals. Paramedics and emergency medical technicians (EMTs) may arrive in ambulances, their personal vehicles, or from another agency. They have control of all aspects of patient care, as assigned by the medical officer or incident commander.
Ground ambulances are assigned to transport patients and personnel to and from the incident scene, emergency departments of hospitals, and designated helipads. Transportation agencies provide buses to transport lightly injured people to hospitals.
Specialized rescue teams may be part of the local fire department or associated with government agencies. These teams specialize in specific types of rescue, such as urban search and rescue (USAR) or confined space rescue. Hazmat teams are responsible for cleaning up and neutralizing hazardous materials at the scene, and they may be specialized CBRNE (chemical, biological, radiological, nuclear, and high-yield explosives) teams.
National Guard units have medical responders trained in mass casualty triage who can be called in to respond to disaster-related incidents. Railways and transportation agencies are notified if an incident involves their tracks or requires them to cease operations in affected areas.
Hospitality Sector: A Massive Job Creator
You may want to see also

Hospitals prepare for a range of disasters, both natural and manmade
Hospitals are increasingly preparing for a range of disasters, both natural and man-made, as the frequency and intensity of mass casualty incidents (MCIs) continue to rise. These incidents can include violence, such as shootings and terrorism, as well as natural disasters like hurricanes, floods, heatwaves, and epidemics. To effectively manage MCIs, hospitals implement comprehensive emergency preparedness plans.
Hospitals with emergency departments have established protocols for MCIs, which include calling in additional medical staff, utilizing spare equipment, and clearing non-acute patients. They may also send doctors to the scene to assist with triage, treatment, and patient transport. Trauma centers play a crucial role, with their levels ranging from Level 1 to Level 4, each providing varying degrees of care and resources.
To streamline disaster response, hospitals now prefer to train their staff using a basic, all-encompassing plan. This plan can be adapted based on the specific incident and local risk factors. For example, in the case of an epidemic, an infectious disease expert would be a key member of the response team, while a hazardous material incident would require someone knowledgeable about chemical, biological, or radioactive agents. During an MCI, job titles become less important, and the focus shifts to utilizing each individual's capabilities to meet the needs of the moment.
In addition to hospitals' internal preparations, external agencies and responders play a crucial role in managing MCIs. These include certified first responders, emergency medical services, paramedics, and emergency medical technicians (EMTs). Mutual aid ambulance services, first responder units, and EMS personnel facilitate patient transportation and evacuation. Specialized rescue teams, such as urban search and rescue (USAR) or confined space rescue teams, may also be involved, along with Hazmat teams for handling hazardous materials.
To optimize patient care, hospitals use simulation models to evaluate their disaster plans and identify areas for improvement, particularly regarding the allocation of resources and staff mix. However, challenges remain, as evidenced by a study of a specialty hospital in Vienna, which found that severely injured patients might have to wait longer than medically justifiable limits for lifesaving surgery, even with increased staff and equipment.
The Dark Knight: Harvey Dent's Escape from Hospital
You may want to see also
Frequently asked questions
A mass casualty incident (MCI) is when hospital resources are overwhelmed by the number or severity of casualties.
Hospitals with emergency departments have mass casualty incident protocols in place, which include calling in more staff, preparing extra equipment, and clearing non-acute patients. Hospitals also train staff on a basic all-encompassing plan, with operational details that depend on the incident and local risk factors.
Multiple agencies are involved in most MCIs, including first responders, paramedics, emergency medical technicians, ground ambulances, and law enforcement. The first available responder squad gauges the extent of the catastrophe and provides a scene report to alert nearby hospitals to determine resource and bed availability.