Hospitals employ a variety of methods to track direct observation privileging, which is the process of evaluating a healthcare provider's behaviour, skills, and procedures within their practice scope. One common approach is the use of provider profiling, which involves systematically compiling and analyzing information related to the healthcare provider's knowledge, professionalism, communication, procedural competency, and patient outcomes. This information is then used by institutional medical staff committees when making decisions on credentialing, privileging, advancement, and promotion. Additionally, hospitals may conduct surveys of expert hospitalists to understand current privileging practices for bedside procedures and how these practices are perceived. Direct observation and proctoring are also utilized during the Focused Professional Practice Evaluation (FPPE) process, which assesses a practitioner's ability to deliver high-quality patient care. Furthermore, hospitals track observation status patients, which can impact patient care and provider workflow. While determining observation status is driven by physician judgment, new metrics help management understand their observation status percentages and make necessary improvements.
| Characteristics | Values |
|---|---|
| Criteria for privileging | Not well described |
| Minimum number of procedures performed | Only half of hospitals require a minimum number of procedures performed to grant initial (48%) and ongoing (52%) privileges for bedside procedures |
| Direct observation of manual skills | Most experts think minimums should exist alongside direct observation of manual skills |
| Use of ultrasound guidance | Nearly universal for paracentesis, thoracentesis, and central venous catheter placement, but only 10% of hospitals required it for initial privileging of these procedures |
| Observation status | Generally limited to 48 hours, but can be longer; should be applied to a well-defined set of specific, clinically appropriate services, including short-term treatments |
| Inpatient status | For serious medical problems requiring highly technical skilled care and a hospital stay of more than a day |
| Provider profiling | Used to systematically compile and analyze information related to the healthcare provider to define their characteristics in areas including knowledge, professionalism, communication, procedural competency, and patient outcomes |
| Focused Professional Practice Evaluation (FPPE) | A standard process mandated by the Joint Commission and used by medical facilities and the medical staff when a practitioner needs a focused plan to assess and ensure the delivery of high-quality patient care |
What You'll Learn
- Hospitals use direct observation to inform privileging decisions, weighing provider profiling
- Direct observation is used to assess a provider's behaviour, skills, and procedures
- Hospitals track observation status patients as a percentage of total days
- Observation status is generally limited to 48 hours, but can be longer
- Observation status patients face higher costs than inpatients

Hospitals use direct observation to inform privileging decisions, weighing provider profiling
Direct observation is a critical component of the FPPE process, as it allows for the assessment of a provider's skills and behaviour in real-time. This can include observing how a provider interacts with patients, their communication skills, and their ability to perform specific procedures. Direct observation can also be used to identify areas where a provider may need additional training or support. For example, if a provider consistently struggles with a particular procedure, direct observation can help identify this issue and inform the privileging decision to provide additional training or supervision.
Additionally, direct observation can be used to assess a provider's professionalism and interpersonal skills. This includes evaluating how they interact with colleagues, their ability to work collaboratively, and their overall conduct in the healthcare setting. Direct observation can also provide insights into a provider's knowledge and decision-making skills. By observing their approach to patient care and treatment decisions, assessors can evaluate their critical thinking, problem-solving, and clinical judgement.
While direct observation is a valuable tool, it is essential to recognise its limitations. Direct observation may not always capture an accurate representation of a provider's skills and behaviour due to factors such as observer bias, variability in performance, or the potential for providers to alter their typical behaviour when being watched. Therefore, direct observation should be combined with other evaluation methods, such as chart reviews, peer evaluations, and patient feedback, to obtain a comprehensive understanding of a provider's competency and privileging decisions.
Furthermore, hospitals must also consider the potential impact of observation status on patients and the organisation. Observation status, distinct from inpatient status, is generally assigned when healthcare providers want to monitor a patient's condition to determine the need for inpatient admission. While it allows for close monitoring, observation status can have financial implications for patients, as it is often classified as outpatient care, resulting in different out-of-pocket costs. Hospitals also face challenges due to inappropriate assignment of observation status, leading to higher costs, bed tie-ups in emergency departments, and interference with efficient service delivery. Therefore, hospitals must carefully manage observation status assignments while adhering to guidelines and regulations to ensure patient care and financial efficiency.
Moving the Deceased: Hospital Protocol for Body Transportation
You may want to see also

Direct observation is used to assess a provider's behaviour, skills, and procedures
Direct observation is a critical component of privileging, which evaluates a provider's behaviour, skills, and procedures within their practice scope at a particular institution. It is a systematic process of compiling and analysing information related to a healthcare provider's characteristics, including knowledge, professionalism, communication, procedural competency, and patient outcomes. Direct observation allows for a comprehensive assessment of a provider's performance and competency, ensuring they deliver high-quality patient care.
The Focused Professional Practice Evaluation (FPPE) is a standard process mandated by the Joint Commission and used by medical facilities to assess and ensure practitioners deliver high-quality patient care. The FPPE process includes various data-gathering modalities, with direct observation being a key component. By directly observing providers, evaluators can assess their manual skills, technical proficiency, and adherence to safety protocols. This helps identify areas of improvement and ensures that providers are practising within the scope of their privileges.
During direct observation, evaluators may focus on several key areas. Firstly, they assess the provider's technical skills and procedures. This includes evaluating the provider's ability to perform specific medical procedures, use medical equipment, and interpret diagnostic results. Secondly, they observe the provider's behaviour and interpersonal skills. This entails evaluating their communication with patients, colleagues, and other healthcare professionals, as well as their ability to work collaboratively within a healthcare team.
Additionally, direct observation allows for the assessment of a provider's decision-making skills and clinical judgement. Evaluators observe how providers analyse patient data, make diagnoses, and determine appropriate treatment plans. This helps ensure that providers are making well-informed and evidence-based decisions in the best interests of their patients. Furthermore, direct observation can also help evaluate a provider's time management skills, organisational abilities, and efficiency in delivering care. This aspect of the observation focuses on the provider's ability to manage their workload, prioritise tasks, and provide timely care without compromising quality.
While the specific details of direct observation may vary depending on the institution and specialty, it remains a valuable tool for assessing a provider's behaviour, skills, and procedures. By utilising direct observation, hospitals can make informed decisions regarding privileging, ensuring that providers are competent, qualified, and capable of delivering safe and effective patient care within their scope of practice.
Pharmacists' Job Satisfaction: Hospital Edition
You may want to see also

Hospitals track observation status patients as a percentage of total days
Observation status is typically assigned when healthcare providers want to monitor a patient's condition to determine if they require inpatient admission. It is considered an outpatient status and can last for multiple days. However, it is generally limited to 48 hours, although hospitals may extend this if deemed necessary. Medicare considers observation an outpatient service, which results in higher out-of-pocket costs for patients compared to traditional inpatient stays.
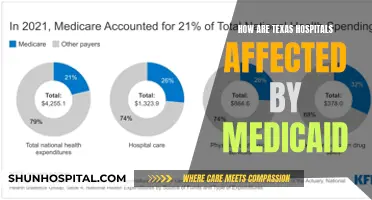
The percentage of observation status patients has been increasing over time. Starting in February 2022, Kaufman Hall's National Hospital Flash Report began tracking the number of observation patient days as a percentage of total days across more than 900 hospitals. This new metric allows hospital management to compare their observation status percentages with the median and identify any significant variances.
By tracking observation status patients as a percentage of total days, hospitals can identify potential issues and make informed decisions to improve patient care and resource allocation. It helps ensure that observation status is appropriately assigned, optimizing patient throughput and efficient delivery of services. This tracking system is a valuable tool for hospitals to manage their operations effectively and provide the best care for their patients.
Behavioral Hospital in Reading, PA: Contact and Services
You may want to see also

Observation status is generally limited to 48 hours, but can be longer
Observation status is generally limited to 48 hours, but there are instances where it can be longer. Observation status is a designation used by hospitals to bill Medicare. It is meant to be a short period for providers to assess whether patients require admission for inpatient care or can be discharged. Typically, this lasts for fewer than 24 hours and rarely spans more than 48 hours. However, the duration of observation stays has increased significantly over the past decade.
The decision to place a patient on observation status is driven by physician judgment and the specific needs of the patient. Observation status is generally applied to a well-defined set of specific, clinically appropriate services, including short-term treatments. If a patient's condition requires additional time to determine the appropriate course of treatment, observation status can be extended beyond 48 hours. This may occur if the physician expects the patient's hospital stay to cross two midnights and is supported by the medical record.
The increase in observation stays has led to the promulgation of the two-midnight rule by Medicare in 2013. This rule provides a clear threshold for inpatient admission, stating that any patient whose hospital stay is expected to cover at least two midnights is generally considered an inpatient. However, this rule has been controversial, and hospitals are required to inform patients of their observation status within 36 hours to comply with the Notification of Observation Treatment and Implication for Care Eligibility Act (NOTICE).
The consequences of observation status designation can be significant for patients, particularly those relying on Medicare for their healthcare coverage. Observation status is classified as outpatient care, which can result in higher out-of-pocket expenses for patients. Additionally, observation status can tie up beds in the emergency department or inpatient units, impacting the efficient delivery of services. Therefore, while observation status is generally limited to 48 hours, it can be extended in certain circumstances to ensure the patient receives the appropriate care.
Amanda Riley's Elaborate Hoax: Faking Hospital Stays
You may want to see also

Observation status patients face higher costs than inpatients
The percentage of observation status patients has increased over the years, and this trend is expected to continue. Observation status patients face higher costs than inpatients due to the differences in reimbursement rates and Medicare coverage. Hospitals receive lower payments for observation status patients, and Medicare Part B does not cover their expenses, resulting in higher out-of-pocket costs for these individuals. Observation stays are reimbursed at lower rates or sometimes not at all, causing hospitals to bear a significant financial burden.
The Centers for Medicare & Medicaid Services (CMS) guidelines define observation status as being applicable to specific short-term treatments or when additional time is needed to determine further treatment plans. However, if a patient is expected to require a hospital stay crossing two midnights, observation status is typically not appropriate. The "two-midnight rule" implemented by Medicare in 2013 reinforced this criterion, but it also led to hospitals favouring observation status to avoid claim disputes.
The distinction between inpatient and observation status significantly impacts patients' financial responsibilities. Observation status patients may not be eligible for Medicare coverage for skilled nursing facility care, resulting in unexpected out-of-pocket expenses. Additionally, observation stays can lead to longer inpatient stays, disrupting efficient service delivery and potentially requiring capital expenditures for additional capacity.
The inappropriate assignment of observation status can be detrimental to both patients and hospitals. Patients may face financial challenges due to higher costs and a lack of Medicare coverage for subsequent skilled nursing care. Hospitals experience financial strain due to lower reimbursement rates and the need for extended observation stays, which can impede their ability to provide timely and appropriate care.
To address these challenges, hospitals can utilise new data and benchmarking tools to improve the accuracy of observation status assignments. Additionally, patients should be proactive in understanding their status and advocating for changes if they believe observation status is inappropriate. Hospitals can also work towards better compliance with CMS guidelines and payers' contractual terms to minimise the negative consequences of observation status assignments.
Securing Hospital Controlled Drugs: Storage Protocols Explained
You may want to see also
Frequently asked questions
Direct observation is part of the Focused Professional Practice Evaluation (FPPE) process, which assesses a provider's behaviour, skills, and procedures within their practice scope at the institution.
Hospitals track direct observation privileging by systematically compiling and analyzing information related to the healthcare provider. This includes knowledge, professionalism, communication, procedural competency, and patient outcomes.
Direct observation privileging helps institutional medical staff committees make decisions on credentialing, privileging, advancement, promotion, acceptance to advanced training, and employment.
There are two main types of privileging practices in hospitals: credentialing and privileging. Credentialing assesses if a provider meets institutional requirements for staff inclusion, such as training, board certification, and malpractice event history. Privileging evaluates a provider's behaviour, skills, and procedures within their practice scope at the institution.