The cleaning and disinfection of medical equipment and tools are essential to prevent healthcare-associated infections (HAIs) and ensure patient safety. Improper cleaning can lead to severe complications and even mortality, as contaminated instruments can harbour harmful microorganisms. To prevent this, hospitals employ various methods, including manual cleaning, the use of detergents, enzymatic products, and disinfectants. Additionally, quality control measures such as routine checks and the use of appropriate personal protective equipment (PPE) are crucial to ensure effective cleaning and disinfection processes.
| Characteristics | Values |
|---|---|
| Cleaning products | Liquid soap, enzymatic cleaners, detergents, alcohol, hypochlorites, ammonia, baking soda, vinegar, Borax |
| Cleaning techniques | Scrubbing, friction, mechanical action |
| Cleaning agents | Neutral detergents with a pH between 6 and 8 |
| Cleaning procedures | Cleaning, disinfection, and sterilization |
| Sterilization | Removal of all microorganisms |
| Disinfection | Removal of most germs |
| Cleaning standards | OSHA, CDC, WHO |
| Cleaning staff | Training on appropriate use of PPE, application, and removal |
| Cleaning equipment | Autoclaves, QUAT-sprayed cloth, QUAT-immersed cloth |
What You'll Learn
- Cleaning solutions: Use appropriate solutions for effective removal of contaminants
- Manual cleaning: Scrub all surfaces, joints, hinges and lumens thoroughly
- Sterilization: Heat or chemical sterilisation eliminates microorganisms
- Maintenance: Regular checks and repairs ensure equipment longevity
- Safety: Proper PPE and handling techniques prevent infections

Cleaning solutions: Use appropriate solutions for effective removal of contaminants
Cleaning is the first step in the decontamination process, and it is crucial for patient safety and the prevention of healthcare-associated infections (HAIs). It involves removing visible dirt, debris, organic matter, and other contaminants from medical equipment and surfaces.
To ensure effective removal of contaminants, it is essential to select the appropriate cleaning solutions. Detergents and water are commonly used for cleaning surfaces and non-critical items, such as blood pressure cuffs and crutches. For surgical instruments, water, detergents, or enzymatic products are often used. However, it is important to choose cleaning solutions specifically designed for medical instruments, as recommended by the manufacturer. These solutions should effectively break down organic material without causing damage to the instruments.
When dealing with blood spills or contamination by blood or body substances, prompt removal and surface disinfection are crucial for infection control. A dilution of sodium hypochlorite (household bleach) can be effective for blood spills. Hypochlorites are also widely used in healthcare settings for spot disinfection of countertops, floors, and equipment.
Alcohol, particularly ethanol or propanol, is commonly used for disinfecting medical equipment such as thermometers, stethoscopes, and external surfaces of ventilators and ultrasound instruments. However, alcohol is not recommended for sterilizing medical and surgical materials as it is not sporicidal.
For reusable cleaning cloths and mops, regular decontamination is essential to prevent the transfer of contaminants. Laundering these items in hot water (70–80°C for 10 minutes) is recommended. Additionally, some hospitals are adopting new mopping techniques using microfiber materials, which require specific disinfectants to avoid damage.
Disease Outbreaks: Financial Impact on Hospitals
You may want to see also

Manual cleaning: Scrub all surfaces, joints, hinges and lumens thoroughly
Manual cleaning is a critical step in the decontamination process, and it is essential to follow proper procedures to ensure patient safety. Before beginning the manual cleaning process, put on all required PPE to avoid any contamination. This includes gloves and, in some cases, a respirator.
When manually cleaning surgical instruments and medical devices, it is crucial to scrub all surfaces, joints, hinges, and lumens thoroughly. This process involves removing any visible dirt, debris, or organic matter, such as residual blood, tissue, and other organic materials. Inadequate cleaning techniques, such as using the wrong tools or not scrubbing thoroughly, can leave behind contaminants that provide a breeding ground for harmful microorganisms. These microorganisms can lead to surgical site infections and other healthcare-associated infections (HAIs), increasing morbidity, hospital stay durations, and healthcare costs.
To effectively scrub all surfaces and their components, use the correct cleaning solutions and tools. Avoid still brushes, as they can damage instruments. Instead, opt for cleaning solutions specifically designed for medical instruments, ensuring compatibility with the materials of the tools. For example, some cleaning agents may be too harsh and cause corrosion, while others may be ineffective against certain contaminants. Refer to the manufacturer's recommendations to select the appropriate cleaning solutions.
Additionally, when scrubbing, combine the cleaning product with water and apply mechanical action through scrubbing and friction. Most environmental cleaning procedures recommend using neutral detergents (with a pH between 6 and 8) that are easily soluble in warm or cold water. However, for specific areas or materials within the healthcare facility, specialized cleaning products may be more advantageous, such as bathroom or floor cleaners.
Immigrant Health: Hospitals' Role in Education and Access
You may want to see also

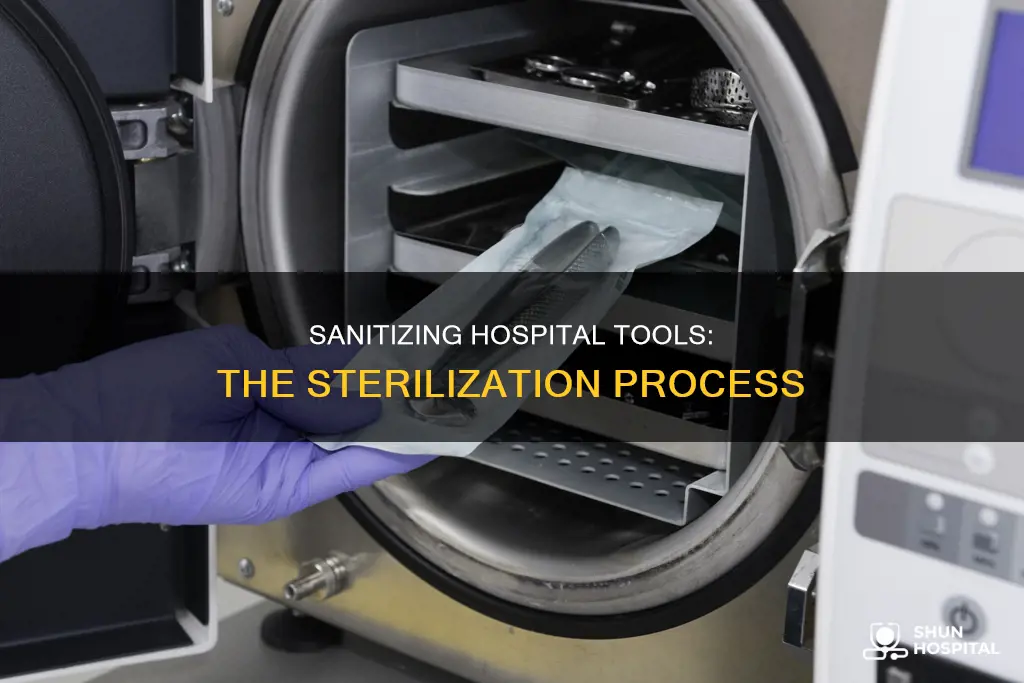
Sterilization: Heat or chemical sterilisation eliminates microorganisms
Sterilization is a critical process in hospitals, aiming to eliminate all microorganisms, including viruses and bacterial spores, from medical tools and surfaces. Heat sterilization and chemical sterilization are two effective methods used to achieve this goal.
Heat sterilization involves applying high temperatures to kill microorganisms. For example, cleaning cloths can be washed in detergent and dried at 80°C for 2 hours to ensure decontamination. This method may pose a fire hazard if the materials being dried contain petroleum-based products or if lint accumulates in the equipment. An alternative heat sterilization technique is autoclaving, which utilizes steam under pressure to sterilize medical instruments.
Chemical sterilization, on the other hand, employs chemical agents to eliminate microorganisms. Hypochlorite, for instance, can be used to disinfect laundry, mop heads, and cleaning cloths in hospitals. A dilution of sodium hypochlorite (household bleach) can be effective for disinfecting surfaces. Additionally, alcohol (ethanol or propanol) is commonly used in healthcare settings for disinfecting equipment such as thermometers, stethoscopes, and external surfaces of ventilators. However, alcohol is not recommended for sterilizing surgical materials as it is not sporicidal.
It is important to note that sterilization is not always necessary for all patient-care items. Hospitals determine whether cleaning, disinfection, or sterilization is required based on the intended use of the item. Disinfection, which removes most germs, can be sufficient in some cases. Proper sterilization techniques are crucial to prevent healthcare-associated infections (HAIs) and ensure patient safety.
Quality control measures, such as routine checks and equipment maintenance, are essential to maintain the effectiveness of sterilization processes. Adhering to standard operating procedures for the preparation, use, and disposal of cleaning products is also vital. Additionally, appropriate personal protective equipment (PPE) should always be worn when handling contaminated items to prevent the spread of infection.
Placenta Retrieval: Your Rights and Requests
You may want to see also

Maintenance: Regular checks and repairs ensure equipment longevity
Maintaining equipment is an essential aspect of ensuring its longevity in hospitals. Regular checks and repairs are crucial to achieving this goal. Here are some detailed insights into the maintenance process:
Firstly, routine checks and validations of cleaning and sterilization equipment are vital. This proactive approach enables the early identification of potential issues, thereby minimizing the chances of equipment failure. It also ensures that cleaning and sterilization processes consistently meet the required standards, reducing the risk of healthcare-associated infections (HAIs).
Secondly, proper handling, transportation, and storage of equipment are essential. Stacking or overcrowding instruments should be avoided, as it can lead to physical damage, such as bending, breaking, or scratching. Such damage can compromise the functionality and sterility of the instruments, affecting their longevity.
Additionally, developing a comprehensive facility monitoring and maintenance schedule is crucial. This schedule should clearly document reusable supplies and equipment, the frequency of inspections, and the staff responsible for maintenance tasks. Adhering to this schedule helps prevent equipment malfunctions and ensures that all equipment is in good working condition.
Furthermore, certain equipment may require specialized maintenance checks. For instance, floor polishers might need to be inspected by qualified personnel according to the manufacturer's instructions. Following manufacturer guidelines helps ensure that specific equipment requirements are met, prolonging the equipment's lifespan.
Lastly, proper training of cleaning staff is essential. They should be well-versed in the appropriate use, application, and removal of required personal protective equipment (PPE) for all environmental cleaning procedures. This training helps ensure the safety of staff and prevents the spread of contamination during cleaning processes. By investing in regular maintenance and adhering to stringent protocols, hospitals can extend the lifespan of their equipment, ultimately contributing to improved patient care and outcomes.
Choosing the Right Hospital for Childbirth
You may want to see also

Safety: Proper PPE and handling techniques prevent infections
In a healthcare setting, personal protective equipment (PPE) and proper handling techniques are crucial for preventing infections and ensuring patient safety. Here are some ways that proper PPE and handling techniques contribute to infection prevention:
Hand Hygiene
Hand hygiene is an essential measure to prevent infections in hospitals. Proper handwashing techniques, including the use of warm water, antiseptic or antimicrobial soap, and disposable towels, are critical for effectively removing microorganisms and preventing their spread. Alcohol-based hand rubs are also recommended as an effective method for hand hygiene.
Personal Protective Equipment (PPE)
PPE is specialized clothing or equipment designed to protect the wearer's body from infection and potential safety hazards. It acts as a barrier, covering the wearer's personal clothing and skin, which may come into contact with infectious materials such as blood or saliva. Examples of PPE include gloves, face masks, protective eyewear, face shields, and protective clothing. Different types of gloves are used for examinations, surgical procedures, and cleaning, with some utility gloves being reusable after sterilization. It is important to change gloves between patients and when they become damaged or compromised.
Instrument Sterilization
Proper sterilization of medical instruments is vital to prevent the transmission of infections. This includes techniques such as chemical sterilization, autoclaving (steam sterilization), and the use of hot air or chemical disinfectants for sharp instruments. Needles, in particular, should be decontaminated and either destroyed or autoclaved if they are reusable. Glassware should be cleaned carefully and sterilized with dry heat.
Handling and Transportation
Preventing infections also involves careful handling and transportation of medical instruments. Stacking or overcrowding instruments can cause physical damage, compromising their functionality and sterility. An Instrument Management System (IMS) is recommended as it keeps instruments within a cassette throughout the reprocessing, avoiding contamination and sharps injuries.
Surface Disinfection
Hospitals should adhere to disinfection protocols for housekeeping surfaces, especially when contaminated by blood or body substances. Detergents, water, or EPA-registered hospital disinfectants are commonly used, depending on the nature of the surface and the type of contamination.
By following these proper PPE and handling techniques, hospitals can effectively prevent infections and ensure a safe environment for patients and healthcare workers.
Charity Care: Hospitals' Benefits and Community Impact
You may want to see also
Frequently asked questions
The cleaning process involves removing any visible dirt, debris, or organic matter from medical equipment using water, detergents, or enzymatic products. This is followed by disinfection, which eliminates most germs, and sterilization, which removes all microorganisms.
Improper cleaning can lead to surgical site infections, which increase morbidity, prolong hospital stays, and raise healthcare costs. It can also interfere with instrument functionality, compromising procedure success and patient safety.
Inadequately sterilized instruments can harbor residual blood, tissue, and other organic materials, providing a breeding ground for harmful microorganisms. These contaminants can cause surgical site infections and increase the risk of HAIs (Healthcare-Associated Infections), leading to severe complications and even mortality.
Standard cleaning solutions include liquid soap, enzymatic cleaners, and detergents. Detergents are often used with water to remove organic material, grease, or oil through scrubbing and friction. For environmental cleaning, neutral detergents with a pH between 6 and 8, soluble in warm and cold water, are recommended.
Cleaning staff should be trained in the appropriate use, application, and removal of PPE (personal protective equipment) for all cleaning procedures. Hand hygiene should be performed before wearing gloves and immediately after removal. Additionally, quality control measures, such as routine checks and equipment sterilization, are essential to ensure optimal equipment functioning.







