Pneumonia is an infection of the lungs caused by fungi, bacteria, or viruses. It is a common cause of hospitalization, particularly in babies, young children, and adults over 50, as well as those with weakened immune systems or other health conditions. Hospital-acquired pneumonia, or nosocomial pneumonia, can occur during a hospital stay, especially if the patient is on a ventilator or has recently been discharged. To reduce the risk of contracting pneumonia in a hospital setting, patients can practice good hand hygiene, receive vaccinations, and avoid exposure to sick individuals, if possible.
| Characteristics | Values |
|---|---|
| Type of Pneumonia | Community-acquired pneumonia, Hospital-acquired pneumonia, Ventilator-associated pneumonia |
| Cause | Infection caused by fungi, bacteria, or viruses |
| Risk Factors | Recent hospitalisation, particularly with ventilator use, weakened immune system, exposure to lung irritants, smoking, heavy alcohol consumption, brain disorders affecting the ability to swallow or cough |
| Symptoms | Chest pain, fever, cough, shortness of breath, congestion |
| Treatment | Antibiotics, oxygen therapy, breathing treatments, drainage of fluid from lungs, vaccination, healthy lifestyle habits |
What You'll Learn

Nosocomial pneumonia
Pneumonia is an infection of the lungs caused by fungi, bacteria, or viruses. It is the second most common cause of hospitalizations in the U.S. and can be life-threatening. Pneumonia can be contracted in a hospital setting, and when this happens, it is called nosocomial pneumonia.
Ventilator-associated pneumonia (VAP) is a type of nosocomial pneumonia that occurs when a patient on a respirator or breathing machine inhales food, liquids, spit, or vomit into their lungs and is unable to cough it out, leading to an infection. The bacteria that cause VAP are similar to those that cause community-acquired pneumonia, as well as drug-resistant bacteria that cause hospital-acquired pneumonia.
To reduce the risk of contracting nosocomial pneumonia during a hospital stay, patients can ask their healthcare providers for advice. Some recommended healthy habits include washing hands frequently, quitting smoking, and avoiding secondhand smoke. Additionally, maintaining a healthy diet, exercising, and getting enough rest can help strengthen the immune system and lower the chances of contracting pneumonia.
The treatment for nosocomial pneumonia depends on its severity and the patient's overall health. Patients are typically given fluids and antibiotics through an IV in the hospital. Oxygen therapy or breathing treatments may also be necessary. In some cases, doctors may need to drain fluid from the patient's lungs. A range of antibiotics may be used, depending on the specific type of bacteria causing the infection.
Tijuana's Top-Rated Hospitals: A Comprehensive Overview
You may want to see also

Ventilator use
Ventilator-associated pneumonia (VAP) is a nosocomial infection that affects critically ill patients who have been undergoing mechanical ventilation in the Intensive Care Unit (ICU). It is the second most common nosocomial infection in such patients, affecting up to 20% of them. Eighty-six percent of nosocomial pneumonias are ventilator-associated. In the US alone, there are between 250,000 and 300,000 cases per year, an incidence rate of 5 to 10 cases per 1,000 hospital admissions.
VAP is typically bacterial and from a single organism, although polymicrobial infections are becoming more common. The most common organisms are Staphylococcus aureus (including MRSA) (28.4%), Pseudomonas aeruginosa (25.2%), and other gram-negative bacteria (26.6%). Other pathogens include Streptococcus, Enterobacteriaceae, and Acinetobacter species.
VAP is usually contracted from the inhalation of bacteria through the ventilator circuit, often from contaminated aerosols, condensate, or suction catheters. It can also be caused by the progression of colonisation of the upper airway. Candida species are also associated with VAP, although they rarely cause invasive pulmonary disease. However, patients colonised with Candida species are 1.58 times more likely to develop VAP.
VAP is associated with increased hospital length of stay, higher healthcare costs, and long-term morbidity and mortality. The attributable mortality of VAP is estimated to be around 10% but can range from 0 to 50%, varying with the type and severity of the underlying illness. Treatment failure occurs in a third to two-thirds of cases, with inappropriate antibiotic use being the most common cause.
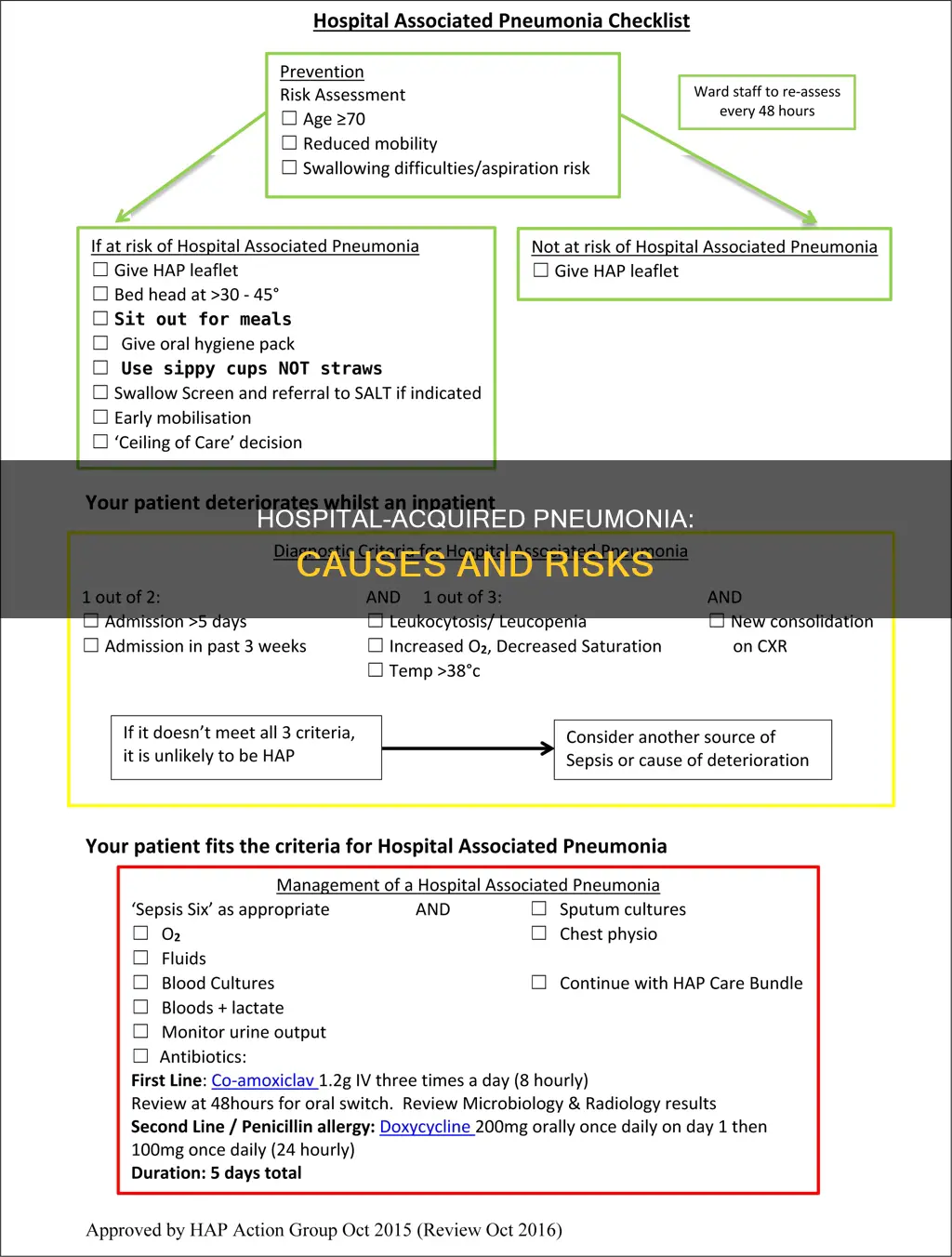
To prevent VAP, guidelines recommend elevating the head of the bed to 45 degrees, which has been shown to result in dramatic reductions in VAP incidence. However, compliance with this simple and cost-free intervention is low.
Rick Grimes: Surviving Hospitalization and the Zombie Apocalypse
You may want to see also

Lung inflammation
Pneumonia is an inflammation of the lungs, usually caused by an infection. It can affect one or both lungs. When an infection causes the air sacs in the lungs (alveoli) and tubes in the airways (bronchioles) to fill with fluid or pus, it can become difficult to breathe.
Pneumonia can be caused by bacteria, viruses, or fungi, and is typically treated with antibiotics. Bacterial pneumonia is more common and severe, and often requires hospitalisation. Viral pneumonia usually resolves on its own and does not require specific treatment.
There are two main ways to contract pneumonia in a hospital:
- Ventilator-associated pneumonia (VAP): This occurs when patients require a respirator or breathing machine during their hospital stay, usually in the ICU. The same types of bacteria that cause community-acquired pneumonia, as well as drug-resistant bacteria, can lead to VAP.
- Hospital-acquired pneumonia: This type of pneumonia is contracted in a hospital setting and can be caused by various bacteria and viruses. It is also known as nosocomial pneumonia.
In addition to the type of pneumonia, an individual's risk factors, general health, and severity of symptoms will determine their treatment plan. Doctors may prescribe antibiotics, antivirals, or other medications, depending on the specific cause of pneumonia.
To reduce the risk of contracting pneumonia during a hospital stay, patients can follow these recommendations:
- Discuss ways to reduce the risk of infection with healthcare providers.
- Practice good hand hygiene by washing hands frequently with soap and water or using an alcohol-based hand sanitiser.
- Avoid close contact and sharing items with others who may have an infectious disease.
- Adopt healthy habits such as quitting smoking, eating healthily, exercising, and getting adequate rest.
Emergency Hydration: Hospital Techniques to Know
You may want to see also

Hospital-acquired bacteria
Pneumonia is an infection of the lungs caused by fungi, bacteria, or viruses. It is the second most common cause of hospitalizations in the U.S. and can be life-threatening. Hospital-acquired pneumonia, also known as nosocomial pneumonia, is a type of pneumonia contracted in a hospital setting. It is caused by bacteria, including drug-resistant bacteria, and is often associated with the use of ventilators or breathing machines in intensive care units (ICUs).
Additionally, aspiration is a common cause of hospital-acquired pneumonia. Aspiration occurs when solid food, liquids, saliva, or vomit enters the trachea (windpipe) and travels into the lungs. If a patient is unable to cough out these foreign substances, their lungs can become infected. This is particularly common in patients with neurological disorders or those who are sedated, such as in intensive care settings.
The risk of contracting hospital-acquired pneumonia can be reduced through various measures. Proper hand hygiene, including frequent handwashing with soap and water or the use of alcohol-based hand sanitizers, is crucial. Patients should also be cautious when in close contact with others, especially those with infectious diseases. Maintaining a healthy lifestyle, including quitting smoking and avoiding secondhand smoke, is essential as smoking damages the lungs and increases the risk of infection.
Furthermore, it is important to get vaccinated against infections that can cause pneumonia, such as the pneumococcal, flu, RSV, and COVID-19 vaccines. Treating any existing infections or health conditions is also vital, as they can weaken the immune system and increase susceptibility to pneumonia. Patients should not hesitate to discuss infection prevention measures with their healthcare providers during their hospital stay.
Profit-Seeking Hospitals: Making Money, Saving Lives?
You may want to see also

Risk factors
Pneumonia is an infection of the lungs caused by fungi, bacteria, or viruses. It is a common cause of hospitalisation, particularly among certain high-risk groups.
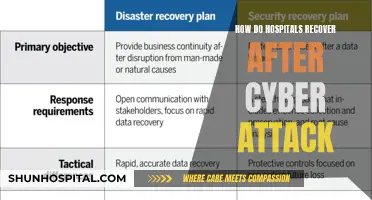
Hospital-acquired pneumonia
Hospital-acquired pneumonia, also known as nosocomial pneumonia, is a type of pneumonia contracted in a hospital setting. It is categorised as ventilator-associated pneumonia (VAP) if the infection is associated with the use of a ventilator or breathing machine. The risk factors for VAP include the use of a ventilator, as well as the presence of drug-resistant bacteria that cause hospital-acquired pneumonia.
Underlying health conditions
People with underlying health conditions are at a higher risk of contracting pneumonia. This includes individuals with lung conditions such as asthma or chronic obstructive pulmonary disease (COPD), heart disease, diabetes, or a weakened immune system due to conditions like AIDS, chemotherapy, or an organ transplant. Those who have recently been discharged from the hospital or reside in a nursing home are also considered to be at increased risk.
Age
Children under the age of two and adults over the age of 50 are at a higher risk of developing pneumonia due to potentially weaker immune systems.
Lifestyle factors
Lifestyle habits such as smoking and excessive alcohol consumption can increase the likelihood of contracting pneumonia. Smoking damages the lungs and makes it more difficult for the body to clear mucus from the airways. Heavy alcohol use weakens the immune system and increases the risk of aspirating saliva or vomit into the lungs.
Exposure to lung irritants
Regular exposure to lung irritants, including air pollution and toxic fumes, particularly in occupational settings, can increase the risk of pneumonia.
Living environment
Living in a crowded environment, such as a prison or nursing home, can elevate the risk of contracting pneumonia due to potential exposure to infectious individuals.
Infection from others
Pneumonia can be contracted from individuals who have the infection or through viral or bacterial infections in the upper airways.
Aspiration
Aspiration occurs when solid food, liquids, saliva, or vomit enters the lungs instead of being coughed out. This can lead to an infection in the lungs, increasing the risk of pneumonia.
Comparing Hospital Maternity Pricing: What to Know
You may want to see also
Frequently asked questions
Pneumonia is an infection of the lungs caused by fungi, bacteria, or viruses. You can get pneumonia in a hospital by being exposed to these pathogens. For example, if you are on a ventilator or breathing machine, you are at risk of ventilator-associated pneumonia (VAP).
You can reduce your risk of contracting pneumonia in a hospital by getting vaccinated, maintaining good hygiene, and avoiding close contact with infected individuals. It is also important to quit smoking and maintain a healthy lifestyle.
Symptoms of pneumonia can include chest pain, fever, cough, and trouble breathing. In more severe cases, individuals may experience congestion, pale or blue skin, and confusion.