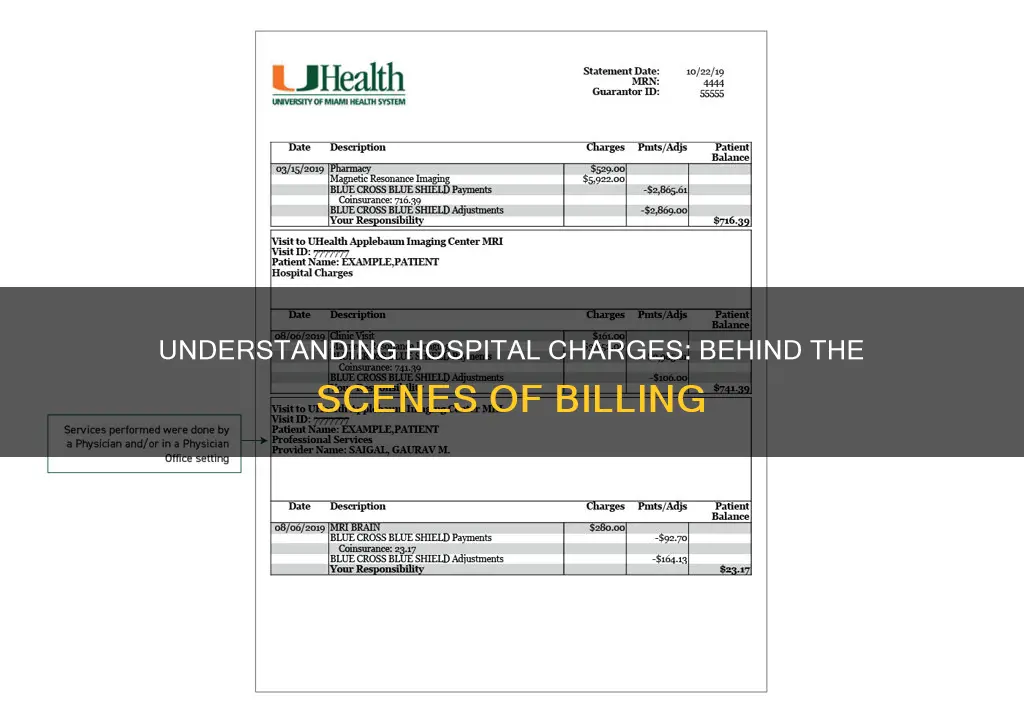
Hospital charges are based on the type of care provided and can differ from patient to patient for the same service. Typically, insurers and patients receive separate bills for hospital care and professional services. Hospital bills comprise facility fees charged by institutions, while professional bills cover the care provided by physicians and other medical professionals. Facility fees are ostensibly overhead charges, but they are not necessarily intended to cover costs specific to the setting or the patient being charged. These fees are becoming more common as hospitals expand their purchase of ambulatory settings and practices, leading to higher overall costs for outpatient care.
| Characteristics | Values |
|---|---|
| Basis of charges | Type of care provided |
| Charge vs expected payment | Charge is the amount billed for a service, expected payment is considerably less |
| Variation in charges | Differs from patient to patient for the same service |
| Reasons for variation | Complications or varying treatments needed due to patient health |
| Professional fees | Charged by doctors |
| Facility fees | Charged by institutions |
| Facility fee range | $0 to thousands |
| Facility fee use case | When hospitals buy and reclassify clinics as "outpatient hospital departments" |
| Insurers' role | Pay nearly 2.5 times Medicare rates for hospital care |
What You'll Learn

Hospital charges are not the same as expected payments
Hospital bills typically consist of two parts: professional fees charged by doctors and facility fees charged by the hospital. Professional fees cover the care provided by physicians and other medical professionals, while facility fees cover the additional costs of providing that care in the hospital. Facility fees are becoming more common as hospitals buy or build outpatient departments and physician practices, leading to higher overall costs for outpatient care. These fees can vary enormously across the country, providers, services, and payers, with insufficient data to understand how insurers address them.
The separation of professional and hospital billing continues even when physicians are employed by a hospital. Patients typically receive two separate bills, one for professional services and one for institutional costs. However, when professionals provide services outside of the hospital, insurers usually require them to charge for their time and practice expenses on the same bill. This allows insurers to negotiate a single combined price for outpatient care.
Hospital charges are based on standard rates for items and services provided, which hospitals are required to make public to promote price transparency and allow patients to make informed decisions about their care. However, actual charges for each patient may vary from the standard charges due to various factors. Patients can use tools like the Shoppable Services Price Estimate Tool or contact their health insurance provider to determine expected out-of-pocket costs, as these may differ from the hospital's listed charges.
Military Medical Care: What Are These Facilities Called?
You may want to see also

Hospitals charge facility fees
Facility fees are separate from professional fees charged by doctors and are billed by the hospital as an institutional bill. These fees can vary enormously across the country, providers, services, and payers, ranging from \$0 to thousands. They are often impossible to anticipate or estimate, and patients might be expected to pay a facility fee for seeing a physician in a hospital-operated clinic or office, even if they never set foot in a hospital.
The separation of professional and institutional billing continues today, even when physicians are employed by a hospital or health system. This traditional separation of billing contributes to the growing public perception that provider prices are too high, as consumers face increased out-of-pocket costs and higher insurance premiums from these extra charges.
In response to the concerns over facility fees, the Biden administration has initiated a proposal to address surprise facility fees. This initiative requires hospitals to make information about facility fees publicly available to consumers, with the goal of increasing transparency and reducing the shock to patients who might be unaware of these charges.
Draining Fluid from Lungs: Hospital Procedure Explained
You may want to see also

Professional fees are charged by doctors
Hospitals set their charges based on the type of care provided, which can differ from patient to patient for the same service. Hospital charges are not the same as expected payments, as hospitals are often paid less than the billed amount. Hospitals are required to publish a list of their standard charges to promote price transparency and public access to information.
Professional fees are an additional cost on top of facility fees, which can increase total hospital service costs by 20-25%. These fees are charged by physicians and other licensed independent practitioners, such as nurse practitioners and physical therapists. Physicians can only charge for services they personally render or supervise and must submit separate bills if multiple doctors are involved. They are expected to be honest and knowledgeable about relevant laws and ethical standards, not providing or charging for unnecessary services.
Facility fees are charged by hospitals for outpatient services and physician office visits within their network, even if the patient never visits the hospital. These fees are meant to cover the high costs of running a hospital, providing 24/7 care, and purchasing new practices. While facility fees vary, they can add hundreds or thousands of dollars to a medical bill, often bearing little relation to the service provided. Patients may be surprised by these fees, especially when doctors' offices are acquired by hospitals, and consumer groups have called for restrictions on their use.
Accreditation Systems: Improving Hospital Performance and Patient Care
You may want to see also

Hospital bills vary from patient to patient
Secondly, hospital bills typically consist of two parts: professional fees charged by doctors and facility fees charged by the hospital institution. Professional fees cover the care provided by physicians and other medical professionals such as nurse practitioners or physical therapists. Facility fees, on the other hand, cover the overhead costs of providing that care in the hospital, including supplies, special equipment, exam rooms, nurses, and support staff. These fees are often billed separately, and their amounts can vary significantly across different hospitals, outpatient clinics, and payers.
Additionally, hospitals are required by law to charge facility fees, but these fees may be higher or lower depending on the specific services provided. The consolidation of hospitals acquiring or building outpatient departments and physician practices contributes to higher prices for patients. This allows hospitals to charge "hospital facility fees" even if the patient never physically enters the hospital campus. The range of these fees can vary from $0 to thousands, and they often appear unrelated to the level of care received.
Furthermore, hospitals with more market power can demand higher prices from private health insurers, which can result in price hikes for patients. The complexity of reimbursement schemes and the variation in how different insurers address facility fees also contribute to the variability in patient billing.
Lastly, the finalized rule from the Centers for Medicare and Medicaid Services (CMS) mandates hospitals to establish, update, and publish a list of their standard charges to promote price transparency. However, these listed standard charges may not always reflect the actual charges for each patient due to various factors influencing the final cost.
Effective Blood Spill Cleanup in Hospitals: A Step-by-Step Guide
You may want to see also

Private insurers pay more than Medicare rates
Hospitals charge private insurers more than Medicare rates. A new report from Rand Corp. revealed that hospitals charged private insurers 254% more than Medicare rates in 2022. This is an increase from 2018, when private insurers paid 222% of Medicare prices, and 2019, when they paid 235%. The difference between private and Medicare rates was greater for outpatient than inpatient hospital services, which averaged 264% and 189% of Medicare rates, respectively. Private insurers paid nearly double the Medicare rates for all hospital services (199% of Medicare rates, on average), ranging from 141% to 259% of Medicare rates across various studies.
The high prices charged to private insurers ultimately mean that patients will also end up paying more, either directly, in the form of higher copays or out-of-pocket payments, or indirectly, in the form of smaller paychecks. According to Brian Briscombe, a health care cost analyst at Rand Corp., about 160 million people in the US get their health insurance through their jobs. He further explains that if an employer pays less for healthcare, they can pay their employees more. In 2022, hospital services accounted for 42% of healthcare spending for people with private health insurance, and price hikes from hospitals were a significant contributor to the rise in the average amount spent per person.
The prices charged to private insurers vary widely among states. Hospitals in Arkansas, Iowa, Massachusetts, Michigan, and Mississippi charged private insurance prices below 200% of what Medicare would have paid. On the other hand, California, Florida, Georgia, New York, South Carolina, West Virginia, and Wisconsin charged private insurance prices above 300% of Medicare rates. The price discrepancies are attributed to the enormous pricing power that hospitals wield. If a hospital has limited competition in a region, it can often charge patients and insurers higher prices.
The separation of professional and institutional billing also contributes to higher costs for patients. Insurers and patients receive separate bills for professional and institutional fees. Professional fees cover the care provided by physicians and other medical professionals, while institutional fees cover the additional costs of providing that care in a hospital. When professionals provide services outside of a hospital, insurers typically require them to charge for their time and other practice expenses, such as rent and equipment, on the same bill. This allows insurers to negotiate a single combined price for the total episode of outpatient care. However, this separation of billing persists even when physicians are employees of a hospital or health system, resulting in higher overall costs for patients.
Hospital charges are based on the type of care provided and can differ from patient to patient for the same service due to complications or varying treatments needed. Hospitals also charge facility fees for care provided in outpatient and physician office settings that they own or control. These fees are ostensibly overhead charges, but they are not necessarily intended to cover costs specific to the setting or the patient being charged. Facility fee charges are becoming more common as hospital systems accelerate their purchase of ambulatory settings and practices, leading to higher overall costs for outpatient care.
Finding Your Nearest Hospital: Quick and Easy Ways
You may want to see also
Frequently asked questions
Hospitals charge a facility fee to cover the costs involved in providing routine and emergency services at that location, including supplies, special equipment, exam rooms, nurses, and support staff. These fees are separate from the fees billed by doctors for their professional services.
Hospital charges are based on the type of care provided and can differ from patient to patient for the same service due to complications or varying treatments needed based on the patient's health.
Facility fees are becoming more common as hospital systems have accelerated their purchase of ambulatory settings and practices, leading to higher overall costs for outpatient care. Large hospital groups can also demand more money from private health insurers, and facility fees vary enormously across the country, providers, services, and payers.