The frequency with which hospitals report to the Centers for Medicare & Medicaid Services (CMS) varies depending on the specific reporting requirements and programs. CMS and hospitals work collaboratively to publicly report hospital quality performance information on Care Compare on Medicare.gov and the Provider Data Catalog. This includes data on hospital outpatient facilities, imaging efficiency, emergency department processes, and surgical care. CMS also collects data on patient experiences through the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. In addition, hospitals are required to report infections that meet specified criteria to the National Healthcare Safety Network (NHSN), which is used for tracking healthcare-associated infections and guiding infection prevention activities. CMS offers detailed guides and training on how to run and interpret the reports, and hospitals can refer to these resources to understand the specific reporting requirements and frequencies for their facilities.
| Characteristics | Values |
|---|---|
| Reporting requirements | An abbreviated list can be found in the "Reporting Requirements to CMS" document. A more detailed list can be found in the "CMS Reporting Requirements and Deadlines" document. |
| Local support | Local Quality Improvement Organization (QIO) or End-Stage Renal Disease (ESRD) Network can provide information on expectations. |
| Reporting programs | Hospital Inpatient Quality Reporting Program (IQR), Hospital Outpatient Quality Reporting Program (OQR), Long Term Care Quality Reporting Program (LTCHQR), Inpatient Rehabilitation Facility Quality Reporting Program (IRFQR), End-Stage Renal Disease (ESRD) Quality Improvement Program (QIP), PPS-Exempt Cancer Hospital Quality Reporting Program (PCHQR) |
| Training | Basic Facility Enrollment and Setup, Data Entry and Analysis, HAI-specific |
| Data validation | Guidance is located on the NHSN Data Validation web page |
| Public reporting | Hospital quality performance information is publicly reported on Care Compare on Medicare.gov and the Provider Data Catalog. |
| Data sources | Medicare-certified hospitals, Department of Defense hospitals, Acute Care Veteran's Hospitals, Critical Access Hospitals, and Children's Hospitals |
| Measures | Over 150 hospital quality measures, including patient experience of care, imaging efficiency patterns, care transitions, emergency department throughput efficiency, care coordination, patient safety, 30-day mortality for heart attack/failure/pneumonia, outpatient imaging efficiency, and surgical processes |
| Goals | Effective, safe, efficient, patient-centered, equitable, and timely care |
What You'll Learn

Hospitals report to CMS via NHSN
Hospitals report to CMS via the CDC's National Healthcare Safety Network (NHSN), a healthcare-associated infection tracking system. The NHSN is the nation's most comprehensive medical event tracking system, used by over 16,000 healthcare facilities across the US, including Puerto Rico and Washington, DC.
The NHSN system is used to track and guide infection prevention activities, with the data being used to determine incentives for performance and to allow members of the public to select providers. The CDC and CMS require that all infections meeting the specified NHSN criteria, and that CMS requires for incentive payments or public reporting purposes, be reported via the NHSN.
The NHSN CMS Requirements webpage provides detailed guides on how to run and interpret the CMS reports. The NHSN Training webpage also offers basic and HAI-specific training courses for users.
It is important to note that any data entered or modified within NHSN after the quarter freeze date will not be reflected in the data posted for Hospital Compare. The frozen data from each quarter are aggregated to produce the measures on Hospital Compare.
In 2020, due to the COVID-19 pandemic, CMS made it optional to submit data for the first and second quarters. Hospitals were still required to enter PC-01 measure data through a web-based tool on a quarterly basis, and aggregate population and sample size counts for each chart-abstracted measure.
Training Proof: Hospitals' Employee Education Verification
You may want to see also

CMS Hospital Inpatient Quality Reporting Program (IQR)
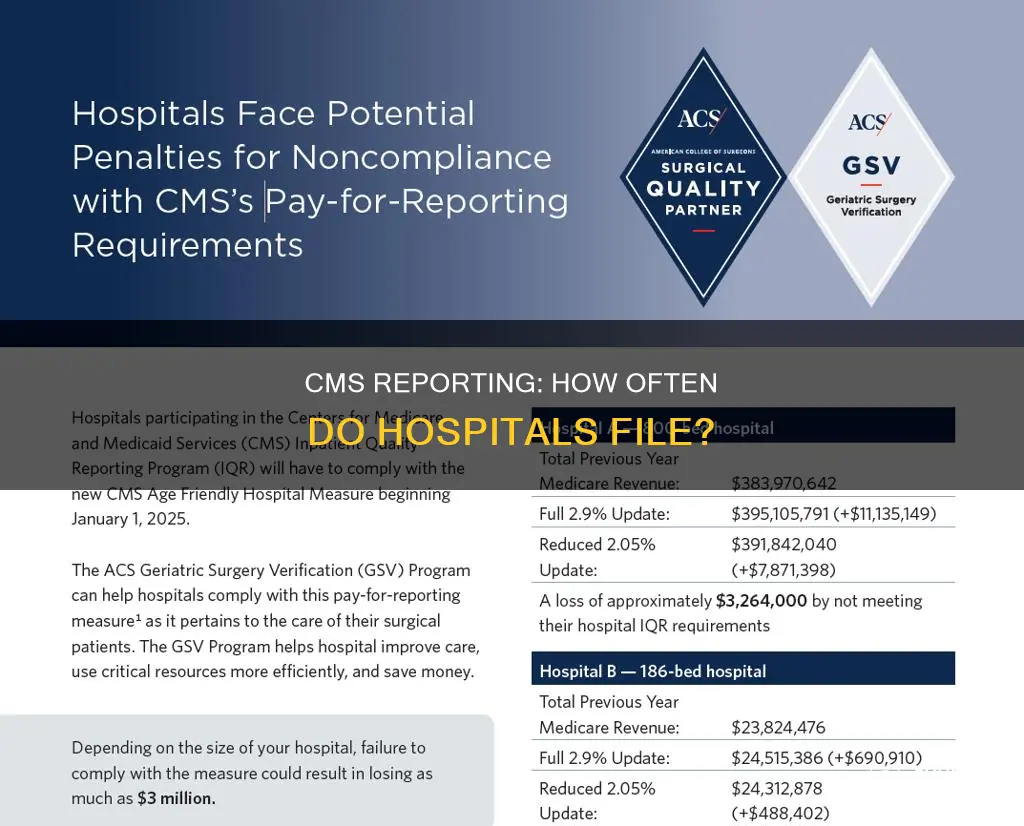
The Hospital Inpatient Quality Reporting (IQR) Program is a pay-for-reporting program for acute care hospitals. Under this program, CMS requires subsection (d) hospitals to submit data on quality measures to CMS each year. The program was developed as a result of the Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003. Section 5001(a) of the Deficit Reduction Act (DRA) of 2005 provided new requirements for the Hospital IQR Program.
The Hospital IQR Program was established by Section 501(b) of the Medicare Modernization Act of 2003 and extended and expanded by Section 5001(a) of the Deficit Reduction Act of 2005. This section of the MMA authorized CMS to pay hospitals that successfully report designated quality measures a higher annual update to their payment rates. Initially, the MMA provided for a 0.4 percentage point reduction in the annual market basket update for hospitals that did not successfully report. The Deficit Reduction Act of 2005 increased that reduction to 2.0 percentage points.
The hospital quality-of-care information gathered through the program is made available to consumers on the Care Compare website. Data collected under the Hospital IQR Program is publicly available to consumers and providers on the Care Compare website. This data transparency helps consumers make more informed decisions about healthcare options and encourages hospitals and clinicians to improve the quality of inpatient care provided to all patients.
CMS first publicly reported data on hospital quality measures on a website called Hospital Compare. Hospital Compare was created through the efforts of Medicare and the Hospital Quality Alliance (HQA). The HQA: Improving Care Through Information, a public-private collaboration, was created in December 2002 to promote reporting on hospital quality of care. The HQA consisted of organizations that represented consumers, hospitals, providers, employers, accrediting organizations, and federal agencies.
CDC and CMS require that all infections that meet the specified NHSN criteria and that CMS requires for incentive payment or public reporting purposes be reported to NHSN. CDC and CMS are issuing this communication to remind all hospitals of the importance of complete and accurate data for purposes of quality of care measurement and improvement.
The Complex Process of Hospital Organ Procurement
You may want to see also

CMS Hospital Compare website
The Centers for Medicare & Medicaid Services (CMS) publicly report hospital quality performance information on Care Compare on Medicare.gov and the Provider Data Catalog. The Hospital Compare website was created through the efforts of Medicare and the Hospital Quality Alliance (HQA). The HQA, a public-private collaboration, was formed in December 2002 to promote the reporting of hospital quality of care. The HQA consists of organisations that represent consumers, hospitals, employers, providers, accrediting organisations, and federal agencies.
The purpose of the HQA is to make it easier for consumers to make informed healthcare decisions and to support efforts to improve quality in U.S. hospitals. Since its inception, many new measures and topics have been displayed on the public reporting sites. For example, in 2005, a ten-measure "starter set" of process-of-care measures was displayed on topics such as heart attack, heart failure, pneumonia, and surgical care.
The Hospital IQR Program was established by Section 501(b) of the Medicare Modernization Act of 2003 and extended and expanded by Section 5001(a) of the Deficit Reduction Act of 2005. The Hospital OQR Program was mandated by the Tax Relief and Health Care Act of 2006. Care Compare on Medicare.gov currently provides quality measure information on process-of-care measures, which show whether or not a health care provider gives recommended care based on guidelines, standards of care, or practice parameters. These measures convert patient medical record information into percentages and/or rates of performance. Providing this information allows consumers to compare the performance of a healthcare provider to other providers in their state and across the nation.
The hospitals displayed on Care Compare are generally limited to Acute Care Hospitals, Acute Care Veteran's Hospitals, Department of Defense Hospitals, Critical Access Hospitals, and Children's Hospitals. Only data from Medicare-certified hospitals are included on Care Compare. Most of the participants are short-term acute care hospitals that will receive a reduction in the annual update of their Medicare fee-for-service payment rate if they do not participate by submitting data or meeting other requirements of the Hospital Inpatient Quality Reporting (IQR) Program.
ACA's Impact: Hospitals' Gains and Pains
You may want to see also

CMS reporting requirements and deadlines
The Centers for Medicare & Medicaid Services (CMS) work collaboratively with hospitals to publicly report hospital quality performance information on Care Compare on Medicare.gov and the Provider Data Catalog. Hospitals displayed on Care Compare include Acute Care Hospitals, Acute Care Veteran's Hospitals, Department of Defense Hospitals, Critical Access Hospitals, and Children's Hospitals.
CMS implements quality initiatives to assure quality health care for Medicare Beneficiaries through accountability and public disclosure. CMS uses quality measures in its various quality initiatives that include quality improvement, pay for reporting, and public reporting. These quality measures are tools that help to measure or quantify healthcare processes, outcomes, patient perceptions, and organizational structure and/or systems that are associated with providing high-quality health care.
CMS regulations require that healthcare facilities adhere to the NHSN protocols, definitions, and criteria and participate in CMS's validation process when selected for participation. CDC and CMS require that all infections that meet the NHSN criteria and that CMS requires for incentive payments or public reporting purposes be reported to NHSN. The NHSN is the nation's most comprehensive medical event tracking system, used by over 16,000 healthcare facilities across all 50 states, Washington, D.C., and Puerto Rico.
Detailed guides for how to run and interpret the CMS reports can be found on the NHSN CMS Requirements webpage. The CDC also offers guidance on the validation of specific event data within facilities, which can be found on the NHSN Data Validation webpage.
Height Measurement Methods in Hospitals
You may want to see also

CMS and NHSN training
The CDC's National Healthcare Safety Network (NHSN) is a tracking system for healthcare-associated infections. It provides data to facilities, states, regions, and the nation, allowing them to identify problem areas, measure the progress of prevention efforts, and work towards eliminating healthcare-associated infections. The NHSN is the most widely used and comprehensive medical event tracking system in the US, with over 16,000 healthcare facilities relying on its data.
To ensure the accuracy and reliability of the NHSN, the CDC and CMS require that all infections meeting the specified NHSN criteria and CMS requirements are reported. This is important for quality of care measurement and improvement, as well as for determining incentives for performance and providing data for the public to select among available providers.
For NHSN users, the CDC recommends completing certain trainings to ensure familiarity with the system and its protocols. New users are advised to start with the basic Facility Enrollment and Setup trainings, along with Data Entry and Analysis trainings. Additionally, all users should complete the HAI-specific trainings relevant to their reporting types, as these cover updated definitions and protocols. These HAI-specific training courses can be found on the respective HAI pages on the NHSN website, and the NHSN Training webpage also provides access to all training courses. It is recommended to complete these trainings once a year, reviewing them at the beginning of each year to stay current with any changes.
To facilitate reporting, the NHSN offers resources such as the NHSN Locations Mapping document, which provides information on setting up locations within a facility. Additionally, the NHSN CMS Requirements webpage offers detailed guides on how to run and interpret CMS reports. The NHSN also provides self-paced trainings, videos, toolkits, FAQs, data validation guidance, and more, to support users in accurately reporting data and contributing to the effectiveness of the system.
Understanding 340B Qualification: A Guide for Hospitals
You may want to see also
Frequently asked questions
CMS (Centers for Medicare & Medicaid Services) works with hospitals to publicly report hospital quality performance information on Care Compare on Medicare.gov and the Provider Data Catalog.
Hospitals are expected to report to CMS annually.
CMS requires that all infections that meet the NHSN criteria be reported. Hospitals must adhere to NHSN protocols, definitions, and criteria and participate in CMS' validation process.
CMS reporting helps measure and improve the quality of healthcare. It also helps determine incentives for performance and allows the public to make informed choices about their healthcare providers.
You can find information on CMS reporting requirements on the CMS website. Detailed guides for running and interpreting CMS reports can also be found on the NHSN CMS Requirements webpage.