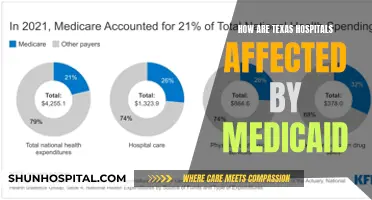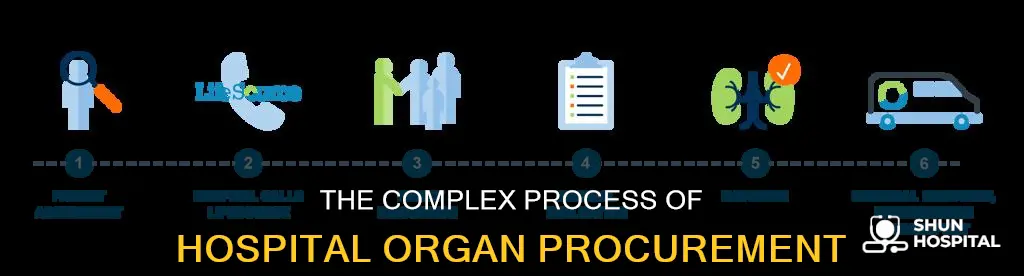
Organ donation and transplantation is a complex process that requires the collaboration of thousands of people. The process typically begins with a decision from an individual to become an organ donor, either before or after their death. In the US, medical specialists from the Organ Procurement and Transplantation Network (OPTN) evaluate the donor's medical status and determine if their organs can be used. The donor's blood type, height, weight, and other data are entered into a national computer system to find the best matches. Organs are then surgically removed and sent to the transplant hospital, where the recipient is waiting. The entire process must be completed within hours to ensure the success of the transplant.
| Characteristics | Values |
|---|---|
| Who can become an organ donor | People who have recently died in a way that didn't damage their organs, often due to traumatic brain injury, brainstem death, or sudden cardiac arrest |
| How to become an organ donor | Register with the Organ Procurement and Transplantation Network (OPTN) in the US |
| How are organs allocated | Based on factors like justice (fair consideration of candidates' circumstances and medical needs) and medical utility (increasing the number of transplants and patient/organ survival) |
| Factors considered for allocation | Blood type, organ size, patient proximity to donor hospital, patient age, and unique organ-specific factors |
| Time constraints | Organs must be transplanted within hours of recovery; hearts and lungs have the shortest preservation time of up to 6 hours |
| Living donors | Yes, living donors can donate organs to recipients |
| Recovery time | It can take 2-6 months to fully recover from organ transplant surgery, requiring a hospital stay of a few days to weeks |
| Organ disposal | Less-than-perfect organs are sometimes discarded due to concerns about poor surgical outcomes and federal standards |
What You'll Learn

Organ donor criteria
Organ donation and transplantation is a complex process that involves many medical and logistical considerations. The donor criteria vary depending on the organ being transplanted and the patient receiving it. Here are the key factors that determine whether someone can become an organ donor:
Death or Brain Death
Most organ donors have recently died in a way that didn't damage their organs, often from a traumatic brain injury, sudden cardiac arrest, stroke, or severe head injury. In these cases, hospitals can preserve their organs after death through mechanical ventilation. Brain death is diagnosed as the irreversible loss of blood flow to the whole brain. After brain death, the donor's body can be supported by artificial means to preserve their organs.
Medical Status and Organ Condition
Specially-trained medical practitioners evaluate the donor's medical status and organ condition to determine their suitability for donation. This includes assessing the size, blood type, and tissue type of the organ, as well as the donor's height, weight, and other relevant data. The condition of the organs is crucial, as some organs, such as hearts and lungs, have a very short preservation time and must be transplanted within hours of recovery.
Donor Registration and Family Consent
In the case of deceased donors, their registration status in a state or national donor registry is considered. If they are registered, their consent to donate is confirmed, and their family is informed. If they are not registered, the donor program staff will consult with the family about the opportunity for donation, answer their questions, and support them through the decision-making process.
Matching with Recipients
The donor's organs are matched with potential recipients based on various criteria, including organ type, size, blood type, genetic compatibility, the recipient's disease severity, time spent waiting, and geographic location. The transplant team at the recipient's hospital also considers staff and patient availability and organ transportation when deciding whether to accept or refuse an organ.
The process of organ donation and transplantation is a collaborative effort involving medical professionals, donor programs, and the donor's family, all working together to save lives and provide hope to those waiting for transplants.
Hospital Financial Records: Keeping Track Securely
You may want to see also

Surgical recovery
Once a potential donor has been identified, they are evaluated to determine their suitability. This includes blood tests to check the donor's tissue type, blood group, and organ function, as well as tests to check for any infections. In the US, medical specialists from the Organ Procurement and Transplantation Network (OPTN) evaluate the donor's medical status and confirm if they are a registered organ donor or consult with their family about the opportunity for donation.
After a suitable donor is found, a specialised surgical team recovers the organs and tissues in a respectful and formal procedure. By federal law, this surgical team is different from the one that cared for the donor. They ensure that the donor's body remains in a suitable condition for the chosen funeral procedure and preserve the organs in special containers.
The recovered organs are then transported to the recipient's transplant hospital, where the recipient awaits surgery. The surgery itself is complex and can take several hours. The transplant team works to ensure the shortest possible preservation time to increase the chances of a successful transplant. Organs can only be preserved for a short time between removal and transplant, and some organs, such as the liver, pancreas, and intestinal organs, need to be transplanted within 12 hours.
After the surgery, the recipient will remain in the hospital for a week or longer. They will then have regular appointments to monitor the functioning of the transplanted organ and adjust to a new routine that includes taking medicines and avoiding certain activities to aid their recovery.
German Hospitals: Migrant Crisis Management
You may want to see also

Organ allocation
In the US, the Organ Procurement and Transplantation Network (OPTN) evaluates potential donors and maintains a national database of registered organ donors. Once a donor is confirmed, their medical status is assessed, and blood tests, x-rays, and ultrasounds are carried out to determine the suitability of their organs for transplantation.
To receive an organ, patients must be evaluated and added to a national waiting list by a transplant hospital. The waitlist considers various criteria, including organ type, geographical location, genetic compatibility, and the recipient's medical condition. When a donor organ becomes available, a dynamic list of potential recipients is generated based on these criteria.
Transplant teams aim for the shortest preservation time to increase the chances of a successful transplant. Organs have a limited time between removal and transplantation, and some, like the liver, pancreas, and intestinal organs, must be transplanted within 12 hours. Therefore, priority is often given to recipients at transplant hospitals closer to the donor hospital.
The allocation process also considers unique factors for each organ type. For example, children often respond better to child-sized organs, so they are typically given first consideration for other children's organs. Blood type and organ size are also critical factors in allocation.
Hospital-Acquired Pneumonia: Causes and Risks
You may want to see also

Transplant surgery
Organ donation and transplantation is a complex, coordinated effort between many parties. It involves removing an organ from a donor and putting it into someone whose organ has failed or is close to failing. Organs that can be transplanted include the heart, lungs, kidneys, liver, skin, bone, tendons, ligaments, parts of the eye, and bone marrow.
The first step in receiving an organ transplant is to get on the national transplant waiting list. Each hospital has its own criteria for accepting candidates for transplant, and the hospital's transplant team will decide whether a patient is a good candidate. The waitlist is a list of candidates registered to receive organ transplants. When a donor organ becomes available, a matching system dynamically generates a list of potential recipients based on criteria such as organ type, geography, genetic compatibility, and the candidate's disease severity.
Transplant teams prefer the shortest possible preservation time to increase the chances of a successful transplant. Organs can only be preserved for a short time between removal from the donor and transplant into the recipient. They are typically transplanted within hours of recovery, and some organs are only viable for six hours after being removed. The donor's heart, for example, is flushed with a special fluid, packed in ice, and transported to the recipient's hospital.
Once the donor organ arrives at the recipient's transplant hospital, the recipient will undergo surgery as soon as possible. Transplant surgery is complex and can take several hours. After surgery, the patient will be in the hospital for about a week or longer. They will then have regular appointments to check how the transplanted organ is working, and will need to take medicines and have regular medical appointments for the rest of their life to prevent organ rejection.
Valley Hospital Las Vegas: Size and Significance
You may want to see also

Post-transplant recovery
The recovery process after organ transplant surgery can be complex and may vary depending on the patient's individual situation. The patient will be taken to the intensive care unit and administered pain medication. They can expect to remain in the hospital for a few days to over a week, with the length of stay depending on the type of organ transplant and whether the donor is living or deceased. For instance, patients receiving a kidney from a living donor usually stay in the hospital for 4 to 6 days, while those receiving a kidney from a deceased donor typically stay for 6 to 10 days.
During their hospital stay, patients will be closely monitored to ensure the proper functioning of the new organ. They will receive IV fluids until they can tolerate food and drinks. Their diet will be gradually progressed from liquids to solid foods. Additionally, their immunosuppression (anti-rejection) medications will be closely observed, and blood samples will be taken to monitor the status of the transplanted organ and other body functions.
After being discharged from the hospital, patients can expect some degree of discomfort and physical limitations. They may need to take time off from work, ranging from a month to two. It is recommended to have someone help with daily activities during this period. Patients should avoid any activity that causes pressure on the transplanted organ and follow their physician's instructions on activity restrictions.
Anti-rejection medications are crucial in preventing the immune system from attacking the transplanted organ. These medications are tailored to each patient and can be given singly or in combination. The doses may change in the early weeks following the transplantation. However, it is important to understand that these medications increase the risk of infections, and patients should be cautious of their surroundings and avoid contact with crowds or anyone with an infection for the first few months.
Tuition Reimbursement: Hospitals' Win-Win Strategy for Retention and Growth
You may want to see also
Frequently asked questions
Hospitals obtain organs from donors. In most cases, organs are donated after a person dies, but in some cases, a living person can donate an organ such as a kidney or part of their liver. Living donors can start the donation process by contacting a donation and transplant center, and deceased donors are usually identified by medical specialists who evaluate the person's medical status. Once a donor is identified, a specialized surgical team recovers the organ in a respectful, formal procedure.
To be eligible for an organ transplant, a patient must be evaluated by a transplant program, which will decide whether to accept them as a candidate. The patient is then added to a national waiting list.
When a donor organ becomes available, a matching system generates a list of potential recipients based on criteria such as organ type, geographic location, genetic compatibility, and the candidate's disease severity. The transplant team at the hospital will then determine whether the organ is a good match for a particular patient.
In addition to organ type and geographic location, other important factors include blood type, organ size, the recipient's disease severity, and time spent waiting. For example, children often respond better to child-sized organs, so they are given first consideration for other children's organs.
Organs can only be preserved for a short time after removal from the donor, and they cannot be frozen or stored long-term. The specific time limit depends on the organ type, with kidneys transplanted within 36 hours and the liver, pancreas, and intestinal organs transplanted within 12 hours.