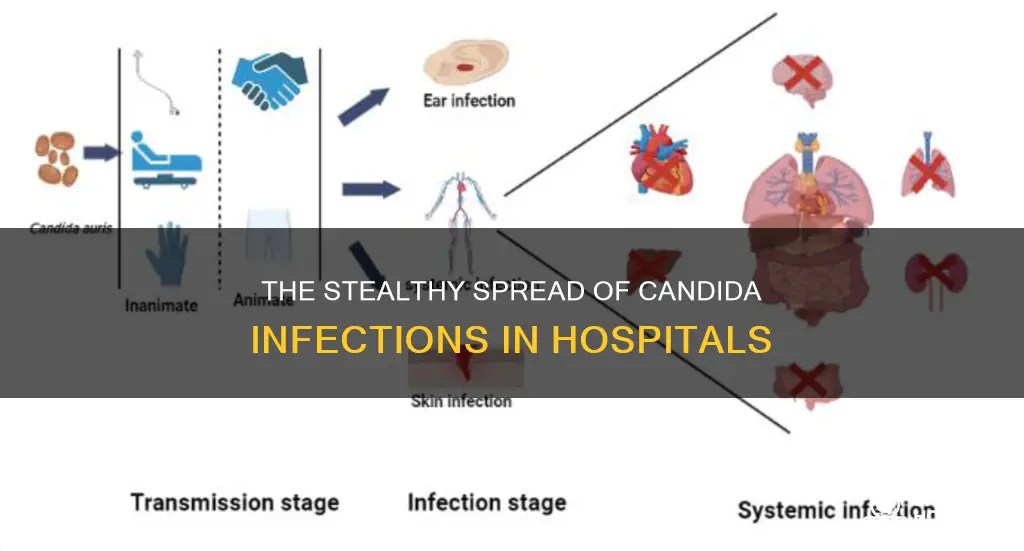
Invasive candidiasis is a serious fungal infection that occurs when a yeast called Candida spreads to a person's internal organs. It is a medical emergency that can lead to life-threatening complications. Candida can spread when a medical device, such as a catheter or peripheral IV, picks up the yeast from a patient's skin and carries it to their organs. It can also be transmitted via healthcare workers' hands or contaminated medical devices. The most common invasive infections spread through the bloodstream, referred to as candidemia. The CDC estimates that around 25,000 patients in the U.S. get candida bloodstream infections annually, with an in-hospital all-cause mortality rate of approximately 30%.
| Characteristics | Values |
|---|---|
| Cause | Overgrowth of Candida yeast, a fungus that lives in parts of the body |
| Transmission | Transmission occurs when Candida yeast enters the body through medical devices like catheters or IVs, or through healthcare workers' hands |
| Risk Factors | Prolonged hospital stays, impaired immunity, critical illness, presence of central venous catheters, use of broad-spectrum antibiotics, total parenteral nutrition, hematologic or solid organ malignancy, neutropenia, burn injury, diabetes mellitus, pregnancy, weak natural immunity, impaired cellular immunity |
| Symptoms | Fever, chills, confusion, low blood pressure |
| Diagnosis | Blood cultures, Beta-D-glucan assay, antifungal susceptibility testing |
| Treatment | Echinocandin antifungals, fluconazole, voriconazole, amphotericin B formulations |
| Prevention | Early diagnosis, improved laboratory methods, understanding drivers and mechanisms of antimicrobial resistance, better hygiene practices |
| Mortality Rate | Approximately 30% in-hospital all-cause mortality in the US |
What You'll Learn
- Candida auris: a recently identified, drug-resistant fungus that spreads between patients
- Transmission via medical devices: Candida can spread when it contaminates medical devices inserted through the skin
- Transmission via healthcare workers: Candida can be transmitted to patients via healthcare workers' hands
- Risk factors: patients with impaired immunity, critical illness, central venous catheters, and broad-spectrum antibiotic use are at higher risk
- Diagnosis: blood cultures are used to diagnose invasive candidiasis, but new diagnostic methods are being developed

Candida auris: a recently identified, drug-resistant fungus that spreads between patients
Candida auris (C. auris), a recently identified drug-resistant fungus, poses a significant threat to global health. Since its emergence in 2009, C. auris has spread rapidly, particularly in healthcare settings, with cases detected in multiple countries, including the United States. This fungus is concerning due to its ability to cause severe and often multidrug-resistant infections, which can lead to high mortality rates.
C. auris typically spreads between patients in hospitals and other healthcare facilities. The fungus can be transmitted through direct contact with healthcare workers' hands or contaminated medical devices, such as catheters and peripheral IVs. Additionally, poor infection prevention and control practices in healthcare facilities have been identified as contributing factors to its spread. The COVID-19 pandemic may have also played a role, as the strain on healthcare systems could have led to a neglect of proper hygiene and disinfection protocols.
To prevent the spread of C. auris, strict adherence to infection control measures is essential. This includes proper hand hygiene by both healthcare personnel and visitors, appropriate use of personal protective equipment, such as gowns and gloves, and effective environmental cleaning and disinfection. Healthcare facilities must also communicate a patient's C. auris status during transfers to ensure seamless transitions and the implementation of necessary infection prevention practices.
While most C. auris infections can be treated with antifungal drugs, some cases have shown resistance to all three main classes of antifungal medications. This multidrug resistance poses a significant challenge in treating affected patients and emphasizes the importance of early diagnosis and effective infection control measures to prevent the spread of this dangerous fungus.
As C. auris continues to spread and evolve, ongoing research and surveillance are crucial to understanding its drivers, mechanisms, and public health impact. By strengthening laboratory capacities and enhancing detection methods, healthcare systems can better identify and manage C. auris infections, ultimately reducing their impact on patient outcomes.
Hospitalization and PIP: Impact and Entitlements
You may want to see also

Transmission via medical devices: Candida can spread when it contaminates medical devices inserted through the skin
Invasive candidiasis is a serious fungal infection that occurs when there is an overgrowth of Candida yeast, which then spreads to a person's internal organs. Candida can spread when it contaminates medical devices inserted through the skin, such as catheters or peripheral IVs. This can happen when Candida yeast from a patient's skin contaminates an intravenous line, allowing the fungus to enter the bloodstream and cause potentially deadly bloodstream infections.
Invasive candidiasis can also occur outside of the hospital setting. For example, a patient who is sent home from the hospital with a central venous catheter they manage themselves may develop an infection. Candida can also be transmitted via the hands of healthcare workers.
Candida auris, a recently identified single-cell fungus, is of particular concern due to its ability to cause invasive infections associated with high mortality rates and its resistance to existing antifungal drugs. It is easily transmissible between patients in healthcare settings and can contaminate surfaces, making it challenging to control.
Healthcare providers play a crucial role in preventing the spread of Candida infections. Early diagnosis and effective treatment are essential to managing invasive candidiasis. Patients with impaired immunity or certain medical conditions are more susceptible to developing invasive Candida infections, and prolonged stays in intensive care units can increase the risk of infection.
The CDC estimates that approximately 25,000 patients in the United States experience Candida bloodstream infections annually, with an in-hospital all-cause mortality rate of about 30%. Antifungal resistance in Candida is an emerging threat, underscoring the importance of early detection and effective prevention methods.
Error Reporting: Saving Hospitals Money
You may want to see also

Transmission via healthcare workers: Candida can be transmitted to patients via healthcare workers' hands
Candida is a yeast that can cause invasive candidiasis, a serious fungal infection that occurs when the yeast spreads to a person's internal organs. Candida auris, a recently identified single-cell fungus, is resistant to existing antifungal drugs and can contaminate surfaces, making it easy to spread from patient to patient and causing outbreaks within and between hospitals.
Candida can spread when a healthcare worker's hands transfer the yeast to a medical device, contaminating it, or directly to a patient. Candida can also spread via contaminated medical devices, such as catheters or peripheral IVs. The fungus can then enter a patient's bloodstream, causing bloodstream infections, which can be deadly.
Healthcare workers should ensure proper hand hygiene and take precautions when handling medical devices to prevent the spread of Candida. This includes wearing gloves and following proper infection control procedures. Additionally, early diagnosis and effective treatment are crucial in managing invasive candidiasis.
Furthermore, the emergence of drug-resistant Candida strains, such as Candida auris, poses a significant challenge to healthcare systems. The development of new therapeutic options and a better understanding of antimicrobial-resistant Candida infections are essential to identify effective prevention methods.
Emergency Treatment: Overdose Protocols and Procedures
You may want to see also

Risk factors: patients with impaired immunity, critical illness, central venous catheters, and broad-spectrum antibiotic use are at higher risk
Invasive candidiasis is a serious fungal infection that occurs when a yeast called Candida spreads to a person's internal organs. It is a medical emergency and can lead to life-threatening complications.
Patients with impaired immunity, critical illness, central venous catheters, and broad-spectrum antibiotic use are at higher risk of contracting invasive candidiasis. Firstly, patients with impaired immunity are more susceptible to invasive Candida infections. This includes those with weak natural immunity, impaired cellular immunity, diabetes mellitus, and pregnancy. These factors can predispose individuals to invasive Candida infections by allowing Candida species to overgrow the normal flora in the body.
Secondly, critical illness, particularly with a prolonged intensive care unit (ICU) stay, is a risk factor. Candida colonisation and infection are closely related and often occur following illness. The risk of Candida colonisation increases during a patient's stay in the ICU, with multifocal colonisation being common among patients who have spent more than seven days in the ICU.
Thirdly, central venous catheters can increase the risk of invasive candidiasis. Candida can spread when it is picked up from the skin's surface by a medical device, such as a catheter, and carried to the internal organs. Contamination can also occur if Candida cells on a person's skin come into contact with an intravenous line, allowing the fungus to enter the bloodstream.
Lastly, broad-spectrum antibiotic use is a risk factor for invasive candidiasis. Antibiotics can disrupt the normal flora in the body, allowing Candida species to overgrow and potentially leading to an invasive infection. It is important to note that other medical conditions and underlying factors may also increase the risk of invasive candidiasis in patients.
Improving Patient Safety: Monitoring Hand Hygiene Compliance
You may want to see also

Diagnosis: blood cultures are used to diagnose invasive candidiasis, but new diagnostic methods are being developed
Invasive candidiasis is a serious fungal infection that occurs when a yeast called Candida spreads to an individual's internal organs. It can cause life-threatening complications and even lead to death. The infection most commonly affects people in hospitals, especially those with weakened immune systems.
Blood cultures are currently used as the primary method to diagnose invasive candidiasis. However, this method has limitations, and new diagnostic techniques are being developed to improve accuracy and speed. The "gold standard" for diagnosis has traditionally been positive blood cultures or histopathology from normally sterile sites. While blood cultures are still widely used, newer culture-independent diagnostic methods are showing promise.
The Beta-D-glucan assay, for example, has been approved as an adjunctive diagnostic tool, but it is not highly specific for Candida. Other non-cultural methods such as T2Candida assays and omics technologies also show potential, but they require further development and validation. The development of more advanced diagnostic techniques is crucial, especially given the emergence of drug-resistant Candida strains.
Determining the species of Candida causing the infection is essential to guide appropriate antifungal treatment. Common Candida species include Candida albicans, C. glabrata, C. krusei, C. tropicalis, and C. parapsilosis. Treatment options for invasive candidiasis are typically limited to systemic antifungals, with echinocandins and fluconazole being the most commonly recommended initial therapies.
In addition to improving diagnostic methods, early recognition of invasive candidiasis is crucial to initiating prompt treatment and improving outcomes. Symptoms can vary depending on the location of the infection but often include fever and chills that do not respond to antibacterial treatment. Some specific signs include "bull's-eye" lesions on the liver or spleen, detectable by imaging, and progressive retinal exudates or vitreal opacities in the case of ocular candidiasis.
Florida Keys Hospitals: How Far Are They?
You may want to see also