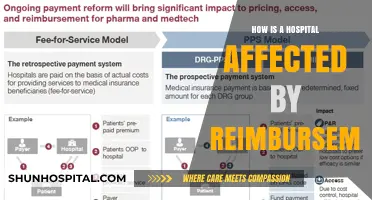
The topic of whether medically necessary dental coverage requires hospitalization is a complex one, with varying policies and interpretations across different organizations and legislation. In the context of Medicare in the United States, there have been calls for expanded coverage of medically necessary dental services, particularly for older adults who are at high risk of poor oral health, which can impact the treatment of other medical issues. While traditional Medicare does not offer broad dental coverage, recent regulatory changes have expanded the types of dental services covered, with new clinical scenarios defined for Medicare payment. Hospitalization may be required for certain dental procedures, especially those involving underlying medical conditions or more severe treatments, and these inpatient services can be covered by Medicare in specific circumstances. However, the interpretation of what constitutes medically necessary dental care and the scope of coverage can vary, and interested stakeholders continue to advocate for expanded access to oral healthcare.
| Characteristics | Values |
|---|---|
| Dental coverage | Granted in limited circumstances, usually in conjunction with jaw surgery |
| Dental services | Covered when they are an "integral part" of inpatient procedures |
| Routine dental services | Not covered by Medicare |
| Dental services for Medicare beneficiaries | Available through Medicare Advantage plans |
| Dental insurance coverage | Covers routine cleanings at 100% |
| Medical insurance coverage | Covers procedures to diagnose or treat a medical condition |
| Non-surgical medical treatments | Covered if they treat a medical condition |
| Surgical treatments | Usually covered as a medical treatment |
What You'll Learn

Dental services covered by Medicare
Medicare does not typically cover dental services like routine cleanings, fillings, tooth extractions, or items like dentures and implants. However, there are certain scenarios where Medicare may cover dental services.
Medicare may cover dental services that are deemed medically necessary and are provided in inpatient (e.g. hospital) and outpatient (e.g. dentist's office) settings. This typically applies to dental services that are inextricably linked to the clinical success of other Medicare-covered procedures or services. For example, dental services required to eliminate a patient's dental infection before an organ transplant may be covered. Similarly, oral exams and dental treatments before procedures like heart valve replacement or a bone marrow, organ, or kidney transplant may be covered.
Medicare may also cover dental procedures required to treat complications that arise during head and neck cancer treatments. This includes dental or oral exams before and during dialysis services for patients with End-Stage Renal Disease (ESRD). Dental ridge reconstruction done during surgery to remove a tumour is another example of a dental service that may be covered by Medicare.
Medicare payment rates for covered dental services vary based on where the services are provided and whether they are performed in a hospital or ambulatory surgery center. For services performed in a Hospital Outpatient Department (HOPD) or Ambulatory Surgery Center (ASC), Medicare pays the facility fee and the professional fee/service to the practitioner.
While the Biden Administration has taken steps to modify Medicare payment policies and expand the types of dental services covered, these changes are expected to benefit a small number of Medicare beneficiaries and do not represent a broad expansion of dental coverage.
Dilated and Hospitalized: When Does it Happen?
You may want to see also

Dental services not covered by Medicare
Medicare does not offer broad coverage of dental services. Under Section 1862(a)(12) of the Social Security Act, Medicare does not pay for items and services in connection with the care, treatment, filling, removal, or replacement of teeth or structures directly supporting the teeth. However, there are certain exceptions where Medicare may cover dental services.
Firstly, Medicare may cover dental services that are deemed medically necessary and are inextricably linked to the clinical success of other Medicare-covered procedures or services. For example, dental services required to eliminate a patient's dental infection before an organ transplant or cancer treatment are covered by Medicare. Dental services covered under this exception include oral exams, tooth extractions, and treatments for oral or dental infections.
Secondly, Medicare may cover dental services provided in inpatient and outpatient settings when the patient requires hospitalization due to their underlying medical condition or the severity of the dental procedure. In these cases, Medicare can pay under Part A and Part B for the hospital services, but not for the dental procedure itself.
It is important to note that the coverage of dental services by Medicare is limited and varies based on the specific circumstances and the location where the services are provided. Medicare payment rates for covered dental services performed in a Hospital Outpatient Department (HOPD) or Ambulatory Surgery Center (ASC) include both the facility fee component and the professional fee/service to the practitioner.
The Biden Administration has recently taken steps to modify Medicare payment policies to expand the types of dental services covered. These changes are expected to benefit a small number of Medicare beneficiaries and do not represent a broad expansion of Medicare coverage of dental services.
Breast Cancer Detection: Hospital Procedures Explained
You may want to see also

Circumstances where hospitalization is required
Hospitalization may be required for dental procedures in specific circumstances, which are typically related to the patient's underlying medical condition or the severity of the dental procedure. Here are some scenarios where hospitalization may be necessary:
Underlying Medical Condition
A person may need to be hospitalized for dental procedures due to their medical condition, which could impact their ability to undergo the procedure in an outpatient setting. For example, individuals with certain medical conditions, such as diabetes, may have an increased risk of infection and may require closer monitoring during and after dental procedures.
Severity of the Dental Procedure
Some dental procedures are inherently more complex and risky, requiring hospitalization to ensure the patient's safety. This could include situations where the patient's clinical status necessitates hospitalization for the safe administration of the dental procedure.
Dental Emergencies
In cases of severe dental emergencies, hospitalization may be required to address life-threatening situations. This could include uncontrolled bleeding, severe pain that does not respond to medication, or significant facial trauma, including broken facial bones.
Inpatient Medical Treatments
Hospitalization for dental procedures is often necessary when dental care is integral to the success of other inpatient medical treatments. For instance, oral exams and dental treatments may be required before certain medical procedures like heart valve replacement, bone marrow or organ transplants, or kidney transplants. Additionally, tooth extractions may be needed to treat mouth infections before cancer treatments such as chemotherapy.
Dialysis and End-Stage Renal Disease
Dental or oral exams are often required before and during dialysis treatments for individuals with End-Stage Renal Disease (ESRD). Hospitalization may be necessary to facilitate these dental exams and ensure optimal oral health before dialysis.
It is important to note that the specific circumstances requiring hospitalization for dental procedures can vary based on individual health needs and the recommendations of dental and medical professionals involved in patient care.
Florida Keys Hospitals: How Far Are They?
You may want to see also

Circumstances where hospitalization is not required
Hospitalization is not always required for medically necessary dental coverage. There are several circumstances in which dental services can be provided in an outpatient setting, such as a dentist's office, without requiring inpatient hospitalization. Here are some examples of circumstances where hospitalization is not necessary:
Dental Infections
Medically necessary dental care may be required to eliminate oral or dental infections before or during certain medical treatments. For example, dental services may be needed to treat an infection before a patient undergoes cancer treatment, such as chemotherapy or radiation therapy. In such cases, hospitalization may not be required, and the dental services can be provided in an outpatient setting.
Pre-Transplant Dental Examinations and Treatments
Dental or oral examinations are often required as part of the comprehensive workup prior to organ transplants, such as kidney or bone marrow transplants. These examinations help identify existing medical problems, reduce the risk of infection, and increase the chances of a successful transplant. In these cases, dental coverage may be provided without the need for hospitalization.
Dental Procedures Related to Jaw Injuries
In some cases, dental procedures may be integral to the treatment of jaw injuries or fractures. For example, tooth extraction may be necessary to prepare the jaw for radiation treatment or to treat a jaw fracture. As long as the dental procedure is directly related to the medical treatment, hospitalization may not be required, and the procedure can be performed in an outpatient setting.
Dialysis Services
Dental or oral examinations and treatments may be necessary for patients receiving dialysis services, especially for those with End-Stage Renal Disease (ESRD). These dental services can help manage oral health complications related to dialysis treatment. Hospitalization is typically not required for these dental examinations and treatments.
Non-Surgical Medical Treatments
Non-surgical medical treatments that are unrelated to traumatic injuries but are linked to a diagnosed medical condition can be billed as medical procedures. This includes emergency treatments for infections or inflammations, incisions and drainage of abscesses, and the use of appliances such as night guards or sleep apnea devices. These treatments can often be provided in an outpatient setting without requiring hospitalization.
It is important to note that the specific coverage and requirements for medically necessary dental care may vary based on the patient's insurance plan, location, and other factors. While hospitalization is not always necessary, the determination of whether a dental procedure requires inpatient hospitalization or can be performed on an outpatient basis depends on the specific circumstances and the patient's medical needs.
The Massive Scale of Global Hospitality
You may want to see also

Other sources of dental coverage
Medically necessary dental coverage may require hospitalization, depending on the patient's underlying medical condition and clinical status, or the severity of the dental procedure. Medicare typically does not cover dental care, except in cases where hospitalization is required for the patient's medical condition or when the dental services are integral to the clinical success of other Medicare-covered procedures.
Now, let's discuss other sources of dental coverage besides insurance:
Dental Coverage in the Health Insurance Marketplace:
The Health Insurance Marketplace offers separate dental plans or health plans that include dental coverage. When comparing plans, you can consider the costs, copayments, deductibles, and services covered. Dental coverage is mandatory for children under 18. The Marketplace dental plans are categorized as high or low, with the latter having lower premiums but higher out-of-pocket costs.
Employer-Provided Dental Benefits:
Many Americans receive dental benefits through their employer or a group program. Large employers are more likely to offer these benefits, and they are more accessible to high-wage workers. These benefits typically follow the 100-80-50 coverage structure, covering preventive care at 100%, basic procedures at 80%, and major procedures at 50%. However, it's important to read the fine print, as some procedures, such as orthodontics, may require additional fees.
Medicaid:
Medicaid programs vary by state, and while most cover dental care for children, coverage for adults may be limited.
Fee-for-Service Dental Plans:
These plans offer a broad network of dental providers, and you pay a percentage of the specified dental service, with the plan covering the rest. There are no annual benefit maximums or deductibles, and some procedures have no out-of-pocket costs.
PPO Dental Insurance:
Preferred Provider Organization (PPO) plans offer a list of preferred dentists within their network, but you can also go out of network for an additional cost. PPO plans typically follow the 100-80-50 coinsurance structure.
DHMO (Dental Health Maintenance Organization):
DHMO plans provide a network of dentists who have agreed to set dental insurance rates, including copays. While this eliminates cost guesswork, you are limited to in-network dentists.
Remember, when considering dental coverage, it's important to review the specific details, exclusions, and limitations of each plan to ensure it meets your unique needs.
Healing Broken Toes: Hospital Treatment Options
You may want to see also
Frequently asked questions
It depends on the procedure and the patient's medical condition. Hospitalization may be necessary for certain procedures due to their severity or the patient's underlying medical condition. However, dental services can be provided in both inpatient and outpatient settings.
Some examples include tooth extractions before cancer treatments or dialysis services, dental examinations before kidney transplants, and dental treatments for infections before organ transplants.
The decision for hospitalization is based on the patient's medical condition and the severity of the procedure. The treating physician typically refers and manages dental care, serving as a gatekeeper for medically necessary dental coverage.