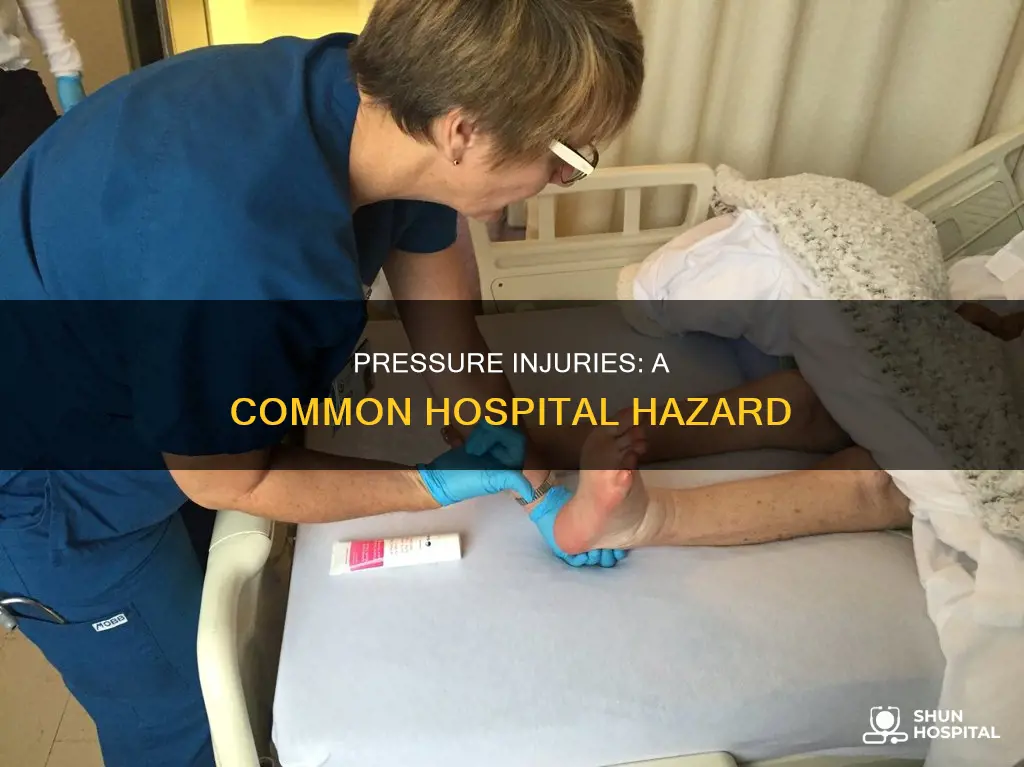
Hospital-acquired pressure injuries, also known as pressure ulcers or bedsores, are a significant concern in healthcare settings, particularly in intensive care units. These injuries are caused by pressure, friction, and moisture on the skin and underlying tissue, especially over bony areas. Patients at risk for pressure injuries often have limited mobility, decreased circulation, and fragile skin. While prevention strategies exist, hospital-acquired pressure injuries remain prevalent, with a 16% incidence rate in intensive care units in the Eastern Mediterranean region. The financial burden of treating these injuries is substantial, and they can also increase patient suffering, length of hospital stay, and mortality rates. As a result, healthcare organizations are motivated to implement preventive measures, such as staff education and adherence to nursing standards, to reduce the occurrence of hospital-acquired pressure injuries.
| Characteristics | Values |
|---|---|
| What | Hospital-acquired pressure injuries, also known as pressure ulcers or bed sores |
| Why | Patients are at risk when they can't move easily, have decreased circulation or fragile skin, have tubes, drains and other healthcare equipment, and have changes in cognitive or bowel and bladder function |
| Where | Intensive care units (ICUs) in hospitals |
| Who | Patients with immobility, decreased circulation, fragile skin, and changes in cognitive or bowel and bladder function are at risk |
| When | During hospitalization, especially in ICUs |
| Prevalence | High prevalence of 16% in ICUs of the Eastern Mediterranean Region; 3.53 pressure ulcers per 100 HACI-eligible Medicare discharges in three states |
| Prevention | The cost of prevention is lower than treatment; prevention techniques include good skincare, helping patients change positions, and using pressure-reducing devices |
What You'll Learn
- Pressure injuries are a major safety concern in intensive care units
- Pressure injuries are largely preventable by adhering to nursing standards
- Pressure injuries are caused by pressure, friction, and moisture
- Hospitals use various techniques to prevent pressure injuries
- The cost of treating pressure injuries is high

Pressure injuries are a major safety concern in intensive care units
Pressure injuries, also known as pressure ulcers or bedsores, are a significant safety concern in intensive care units (ICUs). They are injuries to the skin and underlying tissue caused by pressure, friction, and moisture, often occurring when patients have limited mobility, decreased circulation, or fragile skin. Hospital-acquired pressure injuries are considered largely preventable adverse events, yet they continue to pose a major challenge in ICUs, particularly in the Eastern Mediterranean region, where a study revealed a high prevalence of 16%.
The prevalence of hospital-acquired pressure injuries in ICUs has serious implications for patient well-being and healthcare systems. Pressure injuries can cause significant pain and reduce quality of life, and prolong hospital stays. According to a 2011 German study, patients with pressure ulcers had an average stay of 19 days, compared to 9.9 days for those without, with injuries causing an unnecessary extension of 2.6 days. Longer stays contribute to higher mortality rates and increased healthcare costs. Pressure ulcers are the third most expensive condition to treat after cancer and cardiovascular diseases, accounting for about 4% of Europe's annual healthcare budget.
Various factors contribute to the development of pressure injuries in ICUs. Patients in intensive care often have limited mobility and may be at risk due to decreased circulation or fragile skin. Additionally, they may experience changes in cognitive function, bowel and bladder function, and insufficient nutrient and fluid intake, all of which can increase the likelihood of pressure injuries. The use of tubes, drains, and other medical equipment during hospitalization also poses a risk.
To address this safety concern, hospitals have implemented preventive measures. These include staff training in pressure injury prevention, skin care, regular repositioning of patients, and the use of pressure-reducing devices such as special mattresses and cushions. Despite these efforts, the incidence of pressure injuries remains high, indicating a need for continuous improvement and adherence to nursing standards of care.
The cost of preventing hospital-acquired pressure injuries is significantly lower than the cost of treatment. However, there is a varying level of knowledge among nurses about risk factors and preventive strategies. A hospital in New York addressed this issue by evaluating nurse education and implementing an educational plan to fill knowledge gaps. Comprehensive staff education and adherence to best practices are crucial to reducing the prevalence of pressure injuries in ICUs.
Hospital Financial Records: Keeping Track Securely
You may want to see also

Pressure injuries are largely preventable by adhering to nursing standards
Pressure injuries, also known as pressure ulcers or bedsores, are a significant concern in healthcare settings, particularly in intensive care units. These injuries are caused by pressure, friction, and moisture, leading to wounds and damage to the skin and underlying tissue. Hospital-acquired pressure injuries negatively impact patients' quality of life and increase healthcare costs. Fortunately, these injuries are largely preventable by adhering to nursing standards and implementing specific interventions.
Nurses play a crucial role in preventing hospital-acquired pressure injuries. Firstly, nurses are responsible for identifying patients at risk of developing pressure injuries. This involves conducting routine assessments, including skin status evaluations and risk assessments, to determine patients' likelihood of developing pressure injuries. This identification is a critical first step in prevention.
Once patients at risk have been identified, nurses can implement various preventative strategies. These strategies include routine repositioning of patients, which helps to relieve pressure and improve circulation. Additionally, the use of support surfaces, such as pressure-reducing mattresses, cushions, and other devices, can significantly reduce the incidence of pressure injuries, especially in intensive care units.
Another essential aspect of prevention is moisture management. Maintaining dry skin is crucial in preventing bedsores as moisture can weaken the skin and make it more susceptible to damage. Good skin care practices, including regular skin inspections and the use of appropriate emollients or moisturizers, can help maintain skin integrity and prevent pressure injuries.
Nutritional support is also vital in preventing pressure injuries. Malnutrition risk and insufficient intake of nutrients and liquids can increase the risk of pressure injuries. Nurses can provide nutritional care and ensure patients receive adequate hydration and nutrition to maintain skin health and promote wound healing.
By adhering to these nursing standards and interventions, hospitals can significantly reduce the prevalence of hospital-acquired pressure injuries. Consistent implementation of preventative strategies, such as those mentioned, can improve patient outcomes, reduce healthcare costs, and enhance the quality of care provided.
Great Ormond Street Hospital: Size and Impact
You may want to see also

Pressure injuries are caused by pressure, friction, and moisture
Pressure injuries, also known as bedsores or pressure ulcers, are a major patient safety concern in hospital intensive care units. They are caused by pressure, friction, and moisture acting on the skin and underlying soft tissue. When a patient's skin experiences unrelieved mechanical pressure in combination with friction, shearing forces, and moisture, it can lead to tissue ischemia and eventually necrosis. This results in areas of ulceration and necrosis, commonly known as pressure ulcers or bedsores.
Pressure injuries are particularly common among patients who are older, immobile, or bedridden. Prolonged pressure on the skin, often due to sustained immobility, can cause skin cells to die, leading to the formation of pressure ulcers. Friction, which can be caused by rubbing against clothing or bedding, contributes to pressure injuries by creating local erosion and breaks in the epidermis and dermis layers of the skin. Shearing forces, such as those experienced on an inclined surface, stress and damage supporting tissues, further contributing to the development of pressure injuries.
Moisture plays a significant role in pressure injuries by causing tissue breakdown and maceration. This can be in the form of perspiration, incontinence, or moisture from sweat, urine, or stool. Traction, or the pulling or stretching of the skin, can also worsen pressure injuries. Patients with thinner skin, limited mobility, or sensory deficits are at an increased risk of developing pressure injuries due to their reduced ability to withstand or perceive prolonged pressure.
The prevention and management of pressure injuries are crucial in healthcare settings. This includes the use of specialized mattresses, such as alternating-air mattresses or low-air-loss mattresses, to redistribute pressure and reduce moisture. Friction reduction techniques, such as the use of barrier protectants, can also help. Additionally, regular changes in patient positioning, good skin care, and the use of pressure-reducing cushions and devices are essential for preventing and treating pressure injuries.
The severity of pressure injuries ranges from early-stage nonblanchable skin erythema to late-stage full-thickness skin loss with extensive soft-tissue necrosis. Advanced treatments, including negative-pressure wound therapy, cellular and tissue-based products, and surgical intervention, may be required for neglected or late-stage injuries. Early-stage pressure injuries have an excellent prognosis, while late-stage injuries pose a risk of serious infection and are challenging to heal.
The Massive Scale of Global Hospitality
You may want to see also

Hospitals use various techniques to prevent pressure injuries
Pressure injuries, also known as bedsores, are a major safety concern in hospitals, especially in intensive care units. They are caused by pressure, friction, and moisture, and patients with limited mobility, fragile skin, and decreased circulation are particularly vulnerable. These injuries can cause patient suffering, increase hospital stays, and even lead to premature mortality. Therefore, hospitals employ various techniques to prevent pressure injuries.
One crucial technique is the provision of good skin care. This includes regularly helping patients change positions in bed and using pressure-reducing devices such as special cushions and mattresses. Hospitals also pay close attention to patient nutrition, as insufficient intake of nutrients and liquids can contribute to the development of pressure injuries. At-risk patients are referred to dietitians or nutritionists, and supplemental nutrition is provided as necessary.
Another important strategy is the use of pressure ulcer prevention toolkits, which provide guidelines and best practices for hospitals to follow. These toolkits include information on conducting skin assessments, implementing risk assessments, and developing care plans based on identified risks. Additionally, hospitals ensure that all patient care providers are trained in pressure injury prevention, empowering them to identify high-risk patients and take proactive measures.
Some hospitals also focus on organizational changes to prevent pressure injuries effectively. This involves securing support from senior administrative leadership, assigning clear roles and responsibilities to staff, and implementing standardized protocols for skin and risk assessments. These systemic approaches ensure a cohesive and sustained effort in preventing pressure injuries. Furthermore, hospitals may collaborate with external organizations, such as the Collaborative Alliance for Nursing Outcomes and the National Database of Nursing Quality Indicators, to share data and benchmark their performance against other medical centers.
By employing these techniques and strategies, hospitals strive to minimize the occurrence of pressure injuries, enhance patient safety, and improve overall patient outcomes. Preventing pressure injuries not only reduces patient suffering but also helps shorten hospital stays and lower treatment costs.
Cancer Care in Guyana: Hospital Standards and Availability
You may want to see also

The cost of treating pressure injuries is high
Pressure injuries, also known as bedsores or pressure ulcers, are a significant concern in healthcare, particularly in intensive care units. These injuries, caused by pressure, friction, and moisture, result in wounds to the skin and underlying tissue. Hospital-acquired pressure injuries are largely preventable through adherence to nursing standards of care and evidence-based practices. However, the cost of treating these injuries is substantial and has significant implications for healthcare systems and hospitals.
The financial burden of treating hospital-acquired pressure injuries is considerable. In the United States, the cost of treating these injuries ranges from $3.3 billion to $11 billion annually. A single episode of a hospital-acquired pressure injury can cost hospitals anywhere from $500 to over $70,000. Medicare beneficiaries' claims have shown that chronic pressure injury care can account for about $22 billion. These costs are a significant concern for hospitals, especially as the Centers for Medicare and Medicaid Services (CMS) have reduced reimbursement for hospital-acquired conditions, including pressure injuries.
The high cost of treating pressure injuries is influenced by several factors. Firstly, pressure injuries can lead to extended hospital stays. Research has shown that patients with pressure injuries have longer hospital stays compared to those without, with injuries causing an unnecessary increase in length of stay. This extended stay not only increases inpatient costs but also impacts the availability of beds and resources, affecting the overall efficiency of healthcare facilities.
Additionally, pressure injuries require specialized treatment and resources. The prevention and treatment of pressure injuries demand multidisciplinary collaborations and the utilization of various interventions. These interventions include nutritional support, skin care, use of specialized support surfaces and pressure-reducing devices, and psychological and spiritual support for patients. These resources incur costs for hospitals and healthcare systems, contributing to the overall financial burden of treating pressure injuries.
Furthermore, pressure injuries can lead to complications such as pain, infection, and chronic wounds, which further increase treatment costs. The development of Stage 3 and 4 pressure injuries, indicating more severe and extensive damage, poses significant challenges and expenses for healthcare providers. These advanced stages of pressure injuries require intensive treatment and can contribute to premature mortality in some patients, leading to higher costs for both healthcare providers and society as a whole.
The financial implications of treating hospital-acquired pressure injuries extend beyond the direct costs of treatment. They encompass the utilization of additional staff time, increased readmissions, and the potential need for long-term care or rehabilitation for affected patients. The high cost of treating pressure injuries underscores the importance of prevention and the implementation of evidence-based practices to reduce their occurrence and associated financial burden.
US Hospital Regulation: Who's Watching?
You may want to see also
Frequently asked questions
Hospital-acquired pressure injuries, sometimes called bedsores, are wounds in the skin or underlying tissue caused by pressure, friction, and moisture. They are often found in patients who have difficulty moving, decreased circulation, or fragile skin.
Hospital-acquired pressure injuries are a major safety concern in intensive care units. A 2011 study in Germany found that patients with pressure injuries had a longer hospital stay, with injuries caused by pressure injuries increasing the length of stay by 2.6 days. A systematic review and meta-analysis of intensive care units in the Eastern Mediterranean region revealed a high prevalence of 16%.
Hospitals are implementing various strategies to prevent hospital-acquired pressure injuries, such as providing good skin care, regularly helping patients change positions, and using pressure-reducing devices. Some hospitals are also focusing on educating nurses about pressure injury prevention and risk factors.







