Pneumonia is an infection of one or both lungs caused by bacteria, viruses, or fungi. It can be difficult to distinguish pneumonia from a cold or the flu, and only a healthcare provider can diagnose it. To confirm pneumonia, doctors will first ask about the patient's medical history and symptoms. If symptoms are severe, additional tests may be ordered, including a chest X-ray, blood tests, pulse oximetry, sputum culture, and pleural fluid culture. Treatment depends on the type of pneumonia, the severity of symptoms, and the patient's age and overall health. Most cases of pneumonia are treated at home with rest, fluids, and over-the-counter medications. More severe cases may require hospitalization, with severe bacterial pneumonia being treated with antibiotics.
| Characteristics | Values |
|---|---|
| Confirmation tests | Chest X-ray, Blood tests, Arterial blood gas testing, Sputum culture, Pleural fluid culture, Pulse oximetry, Bronchoscopy, Chest CT scan |
| Treatment | Antibiotics, Vaccination, Healthy diet, Fluids, Rest, Oxygen therapy, Pain medicine, Fever control, Cough-relief medicine |
| Recovery time | 1-2 weeks to a month or more |
What You'll Learn
- A physical exam, including a temperature check, is used to confirm pneumonia
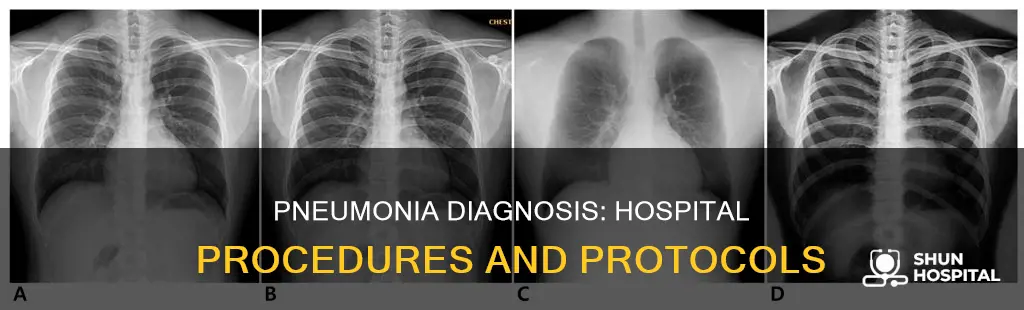
- A chest X-ray can show internal tissues, bones, and organs, including the lungs
- Blood tests can confirm if an infection is present and if it has spread to the bloodstream
- Pleural fluid culture: removing fluid from around the lung to identify bacteria
- Pulse oximetry measures the blood oxygen level

A physical exam, including a temperature check, is used to confirm pneumonia
Pneumonia is an infection of the lungs, caused by bacteria, viruses, or fungi. It can vary in severity, with some cases requiring hospitalisation. Bacterial pneumonia is the most common form and tends to be more serious, requiring medical care. It can be life-threatening, so it is important to seek medical attention if you are experiencing symptoms such as congestion, chest pain, or a high fever.
A physical exam, including a temperature check, is one way to confirm pneumonia. During a physical exam, a doctor will ask about your medical history and perform a lung examination. They may place you in different positions, such as sitting or left and right lateral decubitus, to listen for abnormal sounds consistent with pneumonia, such as rales, rhonchi, or wheezing. This examination can help identify the affected site and determine the severity of the condition. However, it is important to note that a physical exam alone may not be sufficient to confirm pneumonia, and chest radiographs or other diagnostic tools may be necessary.
A temperature check is an important part of the physical exam when assessing for pneumonia. Pneumonia often causes a fever, with temperatures rising above 38°C. In some cases, individuals may also experience hypothermia, with temperatures dropping below 35°C. Monitoring temperature helps in assessing the severity of the condition and guiding treatment decisions.
In addition to the physical exam, physicians may recommend chest radiographs, which are considered the gold standard for confirming pneumonia. These radiographs can identify infiltrates in the lungs, indicating the presence of infection. Other diagnostic procedures may include pleural fluid culture, bronchoscopy, or lung tissue biopsy, especially if initial treatment is not effective.
Overall, a comprehensive approach, including a thorough physical exam with a temperature check, is crucial for accurately diagnosing and managing pneumonia in hospitalised patients.
Donating to Shriners Hospital: A Step-by-Step Guide
You may want to see also

A chest X-ray can show internal tissues, bones, and organs, including the lungs
Pneumonia is an infection of one or both lungs, caused by bacteria, viruses, or fungi. It is a serious condition in which the air sacs fill with pus and other liquids. The diagnosis of pneumonia is usually made based on a patient's recent health history, including surgery, a cold, or travel exposures, and the extent of the illness. A chest X-ray is one of the tests used to confirm a pneumonia diagnosis.
During a chest X-ray, a controlled beam of radiation passes through the body, producing an image on a special type of photographic film. This image provides a detailed view of the internal structures of the chest, including the lungs. The lungs are visible on X-rays due to the difference in density between the air-filled lungs and the surrounding tissues and bones. This contrast allows doctors to examine the lungs for any signs of infection or abnormal changes.
In addition to detecting pneumonia, chest X-rays can also help identify other lung conditions, such as lung cancer, tuberculosis, or pulmonary edema. They can reveal the presence of fluid accumulation, tumours, or other abnormalities in the lungs. Furthermore, chest X-rays can assist in evaluating the heart and its surrounding structures, helping to diagnose cardiac issues or assessing the impact of pneumonia on cardiac function.
While chest X-rays are a valuable diagnostic tool, they have limitations. They cannot directly visualize infections caused by viruses or bacteria, as these organisms are too small to be detected on X-rays. Instead, X-rays show the body's response to the infection, such as inflammation or fluid accumulation. Additionally, chest X-rays may not detect early-stage pneumonia if the changes in the lungs are subtle. In such cases, other diagnostic tests, such as blood tests, sputum culture, or pulse oximetry, may be necessary to confirm the diagnosis of pneumonia.
Urine Drug Tests: Accuracy in Medical Settings
You may want to see also

Blood tests can confirm if an infection is present and if it has spread to the bloodstream
Blood tests are a crucial tool in diagnosing pneumonia and confirming the presence of an infection. Pneumonia is an inflammatory condition caused by an infection in the lungs. It can be caused by various pathogens, including viruses, bacteria, and fungi. The severity of pneumonia symptoms varies depending on the type of pathogen, the patient's age, and their overall health. Bacterial pneumonia, for instance, tends to be more severe and often requires hospitalisation.
Blood tests can help identify the specific germ causing pneumonia. One such test is the blood culture test, which involves analysing a blood sample to identify the bacteria responsible for the infection. This test can also reveal whether the bacterial infection has spread to the bloodstream. Blood culture tests usually take several days to confirm the presence of bacteria, after which targeted treatment can be administered.
Another blood test that can be used is the beta-D-glucan test, which detects the presence of fungal infections. Beta-D-glucan is a component of fungal cell walls, so this test is specific to fungal infections. Additionally, blood tests can be used to detect substances in the blood associated with inflammation, such as procalcitonin and C-reactive protein (CRP). These tests help distinguish between different causes of inflammation and assess the patient's response to treatment.
Furthermore, a complete blood count (CBC) can be performed to evaluate the patient's overall health and immune response. The CBC measures the levels of different blood cell types, including white blood cells, which can indicate the presence of an infection. A high white blood cell count, for instance, suggests that the body is fighting an infection. Additionally, the basic metabolic panel (BMP) is a routine blood test that assesses kidney function, electrolytes, and blood sugar levels, providing valuable insight into the patient's overall health.
In summary, blood tests play a vital role in confirming pneumonia, identifying the causative pathogen, and assessing the patient's overall health and immune response. By utilising various blood tests, healthcare providers can make informed decisions about targeted treatments and closely monitor the patient's response to those treatments.
Understanding Disproportionate Share Hospital Payments: How Are They Made?
You may want to see also

Pleural fluid culture: removing fluid from around the lung to identify bacteria
Pneumonia is an infection that causes inflammation in one or both lungs. It is typically caused by bacteria, viruses, or fungi, with bacterial pneumonia being the most common and severe type. The symptoms of pneumonia can vary from mild to severe, and they depend on the type of pathogen causing the infection, the patient's age, and their overall health.
To confirm pneumonia in a hospital setting, doctors may perform a pleural fluid culture. This procedure involves removing a small amount of fluid from the tissues surrounding the lungs. This process is also known as pleural drainage. The fluid is then analyzed in a laboratory to identify the bacteria causing the pneumonia. This procedure is often carried out when a patient's treatment is not working as expected, and doctors want to investigate whether something else is affecting the patient's airways, such as a blockage.
Pleural fluid culture is a valuable diagnostic tool, especially when used in conjunction with clinical presentation and other tests. However, it is important to note that in some cases, the analysis of pleural fluid may not provide a conclusive diagnosis. The prevalence of negative pleural fluid bacterial cultures is relatively high, with some studies reporting rates of up to 98.53% among patients with pleural effusion.
To guide the diagnosis and treatment of pneumonia, doctors often rely on a combination of tests and procedures. In addition to pleural fluid culture, chest imaging techniques such as X-rays, ultrasounds, and CT scans can help detect the presence of pleural effusions and assess their thickness. In some cases, doctors may also perform bronchoscopy to visually examine the lungs' airways and take fluid samples or lung tissue biopsies for further analysis.
Overall, pleural fluid culture is a valuable tool in the diagnosis and management of pneumonia, especially when used alongside other clinical assessments and imaging techniques.
Hospitals' Emergency Evacuation Plans: Fire Safety Protocols
You may want to see also

Pulse oximetry measures the blood oxygen level
Pulse oximetry is a non-invasive and painless test that measures blood oxygen levels and pulse. It is a quick and easy way to detect even small changes in oxygen levels, which is especially important for patients with pneumonia. The pulse oximeter is a small, clip-like device that is typically attached to a fingertip, but can also be placed on the earlobe or toe. It sends a beam of infrared light through the skin and into the blood in the capillaries, measuring how much light is reflected off the hemoglobin molecules. This information is used to determine the blood oxygen level and heart rate, with results available within seconds.
Pulse oximetry is a standard monitoring technique for patients receiving anesthesia and is also used in emergency departments, hospital wards, and ambulances to assess blood oxygenation in patients with respiratory difficulties. It is particularly useful for patients with pneumonia, as it can help to monitor the effectiveness of oxygen supplementation therapy and detect hypoxemia, or low blood oxygen levels, which is a serious complication of pneumonia. An oxygen saturation level of 95% is considered typical for healthy individuals, while levels below 92% can indicate hypoxemia.
It is important to note that pulse oximetry readings can be affected by various factors, including skin tone, nail polish, and elevation. For example, a 2020 report found that pulse oximetry tests were less accurate in Black patients compared to white patients, with a higher rate of false negatives for hypoxemia. Therefore, it is crucial to be aware of these limitations and consider other diagnostic tools such as blood gas measurements, especially for individuals with darker skin tones.
Pulse oximeters can be purchased for at-home use from pharmacies or online stores, providing a convenient way to monitor one's health. However, it is always recommended to consult a healthcare provider for guidance on interpreting the readings and determining if further testing or treatment is necessary.
Training Proof: Hospitals' Employee Education Verification
You may want to see also
Frequently asked questions
Doctors diagnose pneumonia by asking about the patient's medical history and symptoms. They will also perform a physical examination. If the patient's symptoms are more severe and they have other health issues, the doctor may order additional tests, such as a chest X-ray, blood tests, and pulse oximetry.
Pneumonia symptoms can range from mild to severe. They include congestion or chest pain, a high fever, and a cough with mucus. In more severe cases, the patient's lips and fingertips may turn blue due to lack of oxygen in the blood.
Pneumonia is caused by an infection, most commonly bacteria and viruses, but also fungi. Bacterial pneumonia is the most common type and tends to be more severe.
Treatment depends on the type of pneumonia. Bacterial pneumonia is treated with antibiotics. Most viral pneumonias do not have a specific treatment and will get better on their own. Treatment may also include a healthy diet, rest, oxygen therapy, and medication for pain, cough, and fever control.
Recovery from pneumonia may take some time. Some people recover in one to two weeks, while for others it may take a month or longer. If you've been hospitalized with pneumonia, it may take six to eight weeks to feel back to normal.