Emergency preparedness in hospitals is a critical aspect of healthcare, ensuring the safety and well-being of patients, staff, and the wider community during emergencies and disasters. In recent years, there has been a growing emphasis on hospital emergency preparedness, with federal and state governments implementing various regulations and initiatives to enhance their ability to respond to crises effectively. The development of emergency management standards, the establishment of the Hospital Preparedness Program, and the release of the Emergency Preparedness Rule by CMS in 2016, which sets out requirements for Medicare and Medicaid providers, are all examples of this. Hospitals are now required to have comprehensive emergency plans, including evacuation plans, annual testing, and participation in community-based disaster exercises, to ensure they are equipped to handle both natural and man-made disasters. This topic explores the evolving landscape of hospital emergency preparedness, the challenges faced, and the strategies employed to safeguard public health during critical incidents.
| Characteristics | Values |
|---|---|
| Date of implementation | November 16, 2017 |
| Regulatory body | CMS (Centers for Medicare and Medicaid Services) |
| Purpose | To establish national emergency preparedness requirements to ensure adequate planning for both natural and man-made disasters |
| Scope | Hospitals, skilled nursing facilities, long-term care, group homes, dialysis facilities, and outpatient surgery |
| Requirements | Emergency power and lighting, emergency gas and water supply, evacuation plans, annual testing of emergency preparedness plans, participation in community-based disaster exercises and table-top exercises |
| Compliance | Compliance with CMS regulations is necessary for participation in the Medicare and Medicaid programs |
What You'll Learn
- Hospitals must have emergency power and lighting, with facilities for gas and water supply
- Hospitals must have evacuation plans, though rarely tested due to patient acuity
- Hospitals should conduct a risk assessment to identify potential hazards
- Hospitals should participate in community-based disaster exercises
- Hospitals should work with local emergency response networks to develop preparedness plans

Hospitals must have emergency power and lighting, with facilities for gas and water supply
Hospitals are required to have emergency power and lighting, with facilities for gas and water supply, as part of their emergency preparedness plans. This is to ensure that they can effectively manage and respond to emergency situations, which can vary from internal to external emergencies.
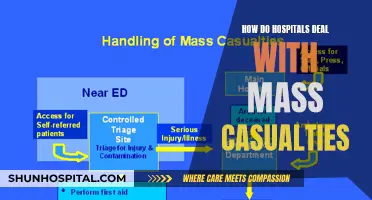
Internal emergencies refer to situations where the emergency condition exists within the hospital facility, such as fire safety and bomb threats. External emergencies occur outside the hospital, such as transportation accidents or natural disasters. In both cases, emergency power and lighting are crucial for maintaining essential functions and patient safety.
Hospitals must have backup power generators and alternative lighting sources to ensure that they can continue to operate in the event of a power outage. This is particularly important for critical care areas such as intensive care units and operating rooms, where uninterrupted power supply is necessary to support life-saving equipment and maintain patient care.
In terms of gas and water supply, hospitals should have access to emergency reserves or alternative sources to prevent interruptions during an emergency. This includes having backup gas cylinders or a central reserve supply, as well as water storage tanks or access to alternative water sources, such as boreholes or water tankers.
To ensure the effectiveness of their emergency preparedness plans, hospitals are required to test and update them annually. This includes conducting evacuation drills and participating in community-based disaster exercises to evaluate their response capabilities and identify areas for improvement. By regularly reviewing and refining their plans, hospitals can enhance their resilience and ability to manage a wide range of emergency situations.
Haven Behavioral Hospital: Frisco Reviews and Complaints
You may want to see also

Hospitals must have evacuation plans, though rarely tested due to patient acuity
Emergency preparedness in hospitals is a critical aspect of healthcare, and while it is not a new concept, its complexity and importance have evolved over time. Hospitals are required to have evacuation plans as part of their accreditation and regulatory requirements, such as the US Centers for Medicare and Medicaid Services (CMS). However, it is rare for these plans to be fully tested due to patient acuity and the potential impact on patient care.
The need to evacuate a hospital can arise unexpectedly, and effective planning is essential to ensure patient safety and well-being. Evacuation plans must consider various internal and external emergency situations, including natural disasters, man-made incidents, and weather-related events. For example, flooding and back-up generator failure led to the unplanned evacuation of several large hospitals, highlighting the importance of preparedness and coordination with other healthcare facilities.
While hospitals are mandated to test their emergency preparedness plans annually, the complexity of patient care and the risk of disrupting essential services pose significant challenges to conducting comprehensive evacuation drills. The focus on patient acuity, which refers to the severity and complexity of patients' medical conditions, takes precedence over testing evacuation procedures. As a result, hospitals rarely conduct full-scale evacuation exercises.
To address this challenge, hospitals are encouraged to develop and maintain comprehensive evacuation plans that can be adapted to various emergency scenarios. The Harvard School of Public Health Emergency Preparedness and Response Exercise Program (HSPH-EPREP) has developed the MDPH Hospital Evacuation Toolkit to assist hospitals in this process. This toolkit provides a step-by-step guide, job action sheets, and customizable spreadsheets that can be tailored to each hospital's unique needs.
Additionally, hospitals can benefit from establishing relationships with other hospital systems and healthcare partners. By fostering these collaborations, hospitals can leverage mutual aid and support during emergencies, as evidenced by the successful evacuation of multiple hospitals through established coalitions. Regular coordination and planning with other medical care facilities in the community are crucial aspects of effective emergency management. While full-scale evacuation drills may be challenging, hospitals can conduct tabletop exercises to evaluate specific disaster processes and procedures without impacting patient care.
Understanding Disproportionate Share Hospital Payments: How Are They Made?
You may want to see also

Hospitals should conduct a risk assessment to identify potential hazards
Emergency preparedness in hospitals is a critical aspect of ensuring community resilience and patient safety during disasters or emergencies. Hospitals are required to conduct risk assessments to identify potential hazards and develop comprehensive emergency management plans. This process involves several key steps and considerations to enhance preparedness and response capabilities.
Firstly, hospitals should identify and assess potential hazards that could directly or indirectly impact their facilities. These hazards can be internal or external to the hospital and may include natural disasters, man-made incidents, accidents, or weather-related events. By considering both direct and indirect hazards, hospitals can anticipate interruptions in utilities, supplies, or staffing and incorporate these factors into their emergency planning.
The risk assessment process should involve a comprehensive analysis of the hospital's vulnerabilities and the likelihood and impact of potential hazards. This includes evaluating the facility's location, infrastructure, patient population, and existing emergency response capabilities. By understanding these factors, hospitals can identify areas of improvement and prioritize resources and efforts effectively.
Additionally, hospitals should involve relevant stakeholders and partners in their risk assessment process. Collaboration with other healthcare providers, emergency management agencies, and community organizations can provide valuable insights and resources for emergency preparedness. By working together, hospitals can establish mutual aid agreements, share best practices, and develop coordinated response plans that enhance overall community resilience.
The risk assessment should also consider the specific needs and challenges of the hospital and its patient population. For example, hospitals serving high-risk or vulnerable populations, such as pediatric or geriatric patients, may require specialized resources and response strategies. By tailoring their emergency plans to their patient demographics, hospitals can ensure that the unique needs of their patients are addressed effectively.
Furthermore, hospitals should regularly review and update their risk assessments to account for changing conditions and emerging hazards. This includes conducting periodic hazard mitigation activities to reduce the likelihood and impact of identified risks. By staying proactive and adaptable, hospitals can enhance their emergency preparedness and response capabilities, ensuring they are well-equipped to handle a diverse range of emergencies.
Hospital Admissions: My Personal Experience and Story
You may want to see also

Hospitals should participate in community-based disaster exercises
Emergency preparedness in hospitals is a critical aspect of ensuring community resilience and patient safety during disasters. Hospitals should actively participate in community-based disaster exercises for several key reasons:
Firstly, hospitals are integral to community emergency response. When a disaster strikes, the impact on the community can be far-reaching, affecting not only individuals but also essential services such as utilities, transportation, and communication. Hospitals, as part of the community fabric, need to be prepared to handle not just patient care but also potential disruptions to their own operations. By engaging in community-based exercises, hospitals can enhance their ability to coordinate with local emergency services, public health departments, and other medical facilities, thereby improving the overall effectiveness of the community's disaster response.
Secondly, community-based disaster exercises provide a unique opportunity to identify and mitigate hazards specific to the hospital's location. Hospitals should strive to anticipate potential direct and indirect hazards, such as those that may affect necessary utilities, supplies, or staffing. For example, flooding and back-up generator failure led to the unplanned evacuation of several large downtown hospitals including New York University Langone and Bellevue Hospital. Through participation in community exercises, hospitals can gain valuable insights into the specific challenges they may face during different types of disasters and work collaboratively with local partners to develop effective mitigation strategies.
Additionally, these exercises enable hospitals to test their emergency preparedness plans and evacuation protocols in a controlled environment. While hospitals are required to have evacuation plans, full-scale testing is rarely conducted due to patient acuity. Community-based exercises provide a platform for hospitals to evaluate their plans, identify weaknesses, and make necessary improvements. This includes ensuring the safety and well-being of patients during an evacuation, which is a complex and time-critical endeavour. By regularly participating in community drills, hospitals can build the expertise and confidence needed to execute successful evacuations when unexpected disasters occur.
Furthermore, community-based disaster exercises foster the development of healthcare coalitions and strengthen relationships with various partners. Coalitions and partnerships are crucial for effective emergency management. Hospitals that nurture relationships with other healthcare providers, response agencies, and community organizations can leverage these connections during exercises to enhance coordination, share resources, and develop comprehensive disaster response strategies. These relationships contribute to the overall resilience of the healthcare system and the community it serves.
Lastly, community-based exercises promote a culture of continuous improvement in emergency preparedness. Hospitals can learn from the experiences and best practices of other organizations involved in the exercises. By evaluating their performance and adopting corrective measures, hospitals can refine their emergency management programs, including planning, organizing, training, equipping, and coordinating responses. This iterative process ensures that hospitals are better prepared to handle not only external emergencies but also internal emergencies, such as fire safety and bomb threat situations, which require a different organizational response.
In conclusion, hospitals play a vital role in community disaster response, and their participation in community-based disaster exercises is essential. Through these exercises, hospitals can enhance coordination with local partners, identify and mitigate location-specific hazards, test and improve their emergency plans, foster valuable coalitions, and continuously refine their emergency management capabilities. By actively engaging in these exercises, hospitals contribute to a more resilient and better-prepared community, ultimately saving more lives and reducing the impact of disasters.
Bacterial Identification: Hospital Strategies and Techniques
You may want to see also

Hospitals should work with local emergency response networks to develop preparedness plans
Emergency preparedness in hospitals is a dynamic and complex process that has evolved over the years, with a growing emphasis on community resilience and coordinated responses. Hospitals play a vital role in emergency management, and their preparedness plans are crucial for ensuring the safety and well-being of patients and the wider community. Here are some reasons why hospitals should actively collaborate with local emergency response networks to develop robust preparedness plans:
Community Resilience and Collaboration:
By working closely with local emergency response networks, hospitals can foster stronger community resilience. This collaboration allows for the development of healthcare coalitions, which include healthcare partners at all levels, such as the Chemical Stockpile Emergency Preparedness Program and the Hospital Preparedness Program. These coalitions provide a unified front in emergency situations, ensuring that healthcare services remain accessible to the community, even in the face of disasters.
Coordinated Response and Resource Sharing:
Emergency situations often require a coordinated response involving multiple entities, including medical and public health organizations, emergency medical services, and medical support services. Hospitals, as key stakeholders, can work with local emergency response networks to establish clear lines of communication and coordination. This coordination facilitates efficient resource sharing, including staffing, supplies, and equipment, which is essential during emergencies that may strain individual hospital capacities.
Hazard Identification and Mitigation:
Hospitals, in collaboration with local emergency response networks, can more effectively identify potential hazards that could directly or indirectly impact their facilities and the surrounding community. This includes natural disasters, man-made incidents, and unintentional accidents. By understanding these hazards, hospitals can actively engage in hazard mitigation strategies, reducing the likelihood and impact of emergencies.
Evacuation Planning:
Developing evacuation plans is a critical aspect of emergency preparedness. Hospitals, in collaboration with local emergency response networks, can establish comprehensive evacuation protocols, ensuring the safe and timely evacuation of patients when necessary. This coordination includes identifying alternative care facilities, transportation methods, and the efficient utilization of resources during evacuations.
Compliance with Regulatory Requirements:
Hospitals are subject to various regulatory requirements, such as the Emergency Preparedness Rule published by the CMS, which mandates specific preparedness measures for Medicare and Medicaid providers. By working with local emergency response networks, hospitals can ensure they meet these requirements, including annual testing of emergency preparedness plans and participation in community-based disaster exercises. This collaboration helps hospitals maintain compliance and access necessary resources during emergencies.
In conclusion, hospitals can enhance their emergency preparedness by actively collaborating with local emergency response networks. This collaboration fosters community resilience, improves coordination, facilitates resource sharing, and ensures compliance with regulatory mandates. By working together, hospitals and local emergency response networks can better protect the health and safety of the communities they serve.
Understanding Hospital Doctor Payment Structures
You may want to see also
Frequently asked questions
Hospitals are required to have emergency power and lighting in some areas and facilities for emergency gas and water supply. They are also mandated to have evacuation plans and test their emergency preparedness plans annually.
The goals of emergency preparedness are to ensure adequate planning for both natural and man-made disasters and to coordinate the response of various entities, including health care provider systems, public health departments, and emergency medical services.
Hospitals are required to test their emergency preparedness plans once a year. This includes participating in an annual community-based disaster exercise and a table-top exercise to evaluate specific disaster procedures.
Smaller hospitals with limited capabilities are encouraged to work with local emergency response networks to develop emergency preparedness plans that consider their limitations. Additionally, hospitals that exceed CMS requirements will remain compliant.